|
�ӹ�����˨��ʱ���ѳ���������
Ů����ֳϵͳ�Ķ����������ڶ��������ӹ������ǹ�Ӧ�ӹ�����Ҫ�������ѳ�������Բ�ʹ��������ӹ��ķ���Ҫ��Ѫ�������ѳ�����ͨ����������dz�ϸС�������н����ѳ������������Ըı䡣�����Ѫ���ӹ�������Ѫʱ�ѳ����������֡�
��������Ӱ���Է����ѳ�����ռ20~30%��88/290����5����69%��37/54�����ѳ����������ӹ�������Ѫ��Ҳ�б�����������Ӱ�ѳ�������Ӱ��Ϊ20%��59/294�����ѳ����������ӹ�������ѪΪ25%��15/59����2����40.3%�ӹ�����-�ѳ��Ǻ�֧���š�6���� �ѳ�����83%������������������������������ǻ��ռ17%���ѳ���Ѫ�������ѳ�������Ѫռ40%���������ӹ�������Ѫ��ռ4%���ӹ��������ѳ��������Ϲ�Ѫ��ռ56%���ӹ�������ӹ�������Ѫ��ռ90%�����ѳ�������Ѫ��ռ10%��7����
�ӹ����������ѳ�������Ѫ
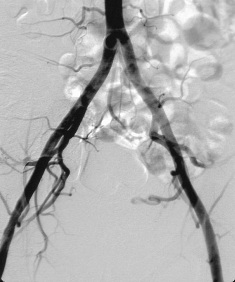
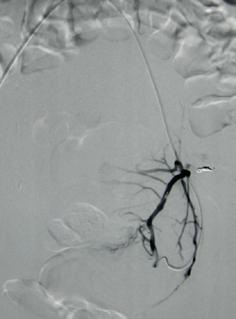
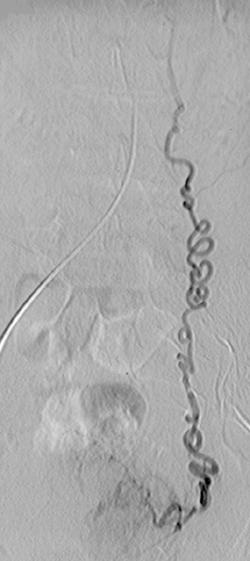
Courtesy M Razavi, USA
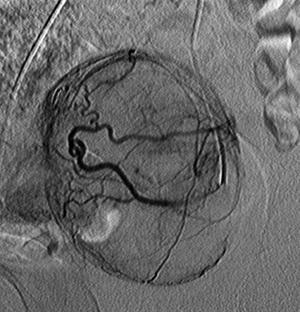
˨�����ѳ�������Ӱ֮һ
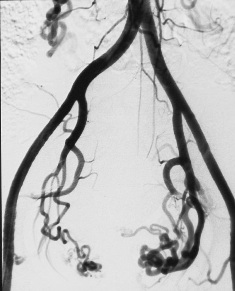
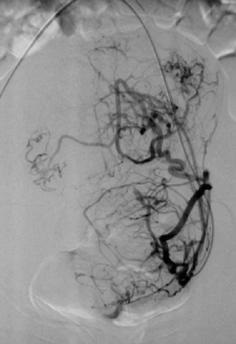
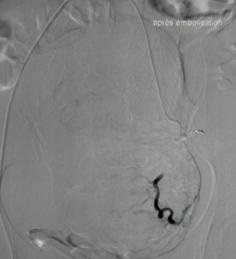
˨�����ѳ�������Ӱ֮��
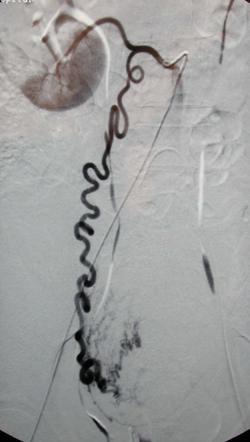
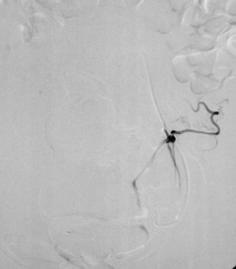
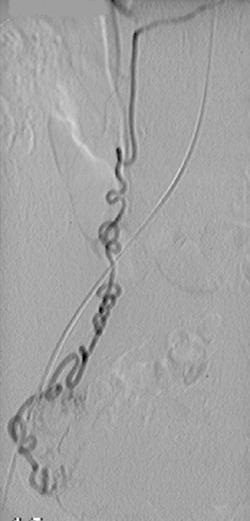
����˨���ѳ���������
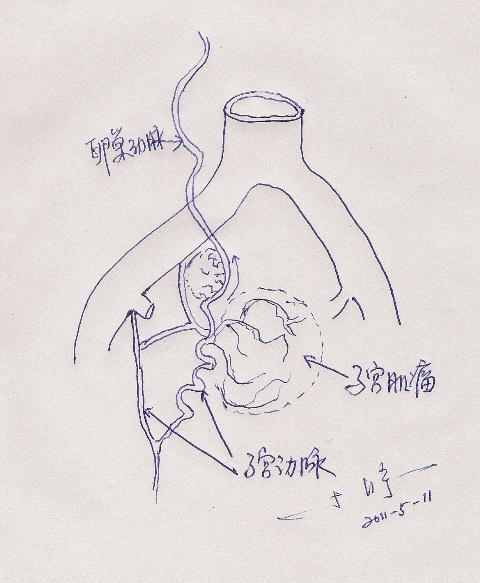
��һЩ�����Ӧ�ر�ע���ѳ��������ܲ����ӹ������Ĺ�Ѫ�����������ǰ��ǻ����������ӹ������г������ʸ����������ѹ�-�ѳ����䣨���ѹ��ף����ѹ��������ͽϴ�Ĺ����ӹ�����[2]���ӹ������쳣��С��ȱ��������ʷ��Ҳ�ᵼ���ѳ������쳣��Ѫ����˨���ӹ�����ʱ��Ѱ���ѳ��������г�ӯ��һ�������ѳ�����Ӧ�ÿ���ֹͣ˨�� / ����˨��������ֱ�� / ʹ������˨�ӱ�������֮Ҫ�����������ѹܺ��ѳ������ˡ���ʱ����ý���MRA����ǰ��ʾ�ѳ�������ע���ӹ��������ѳ��������Ǻ�֧����������ӹ�����˨����ʱ�����Ե��ѳ������ӹ�������Ѫ�����ҵ���˨���ӹ�����û�����ӹ�����ȫ���������ѳ�������˨����ð��ŵ��´ν��С� �ѳ����������ӹ������Ĺ�Ѫ
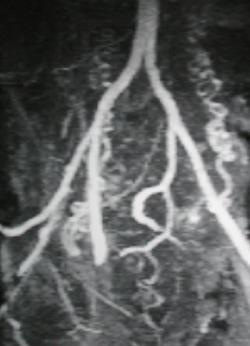
˨��ǰMRA��ʱ�����ṩһЩ�ѳ������������
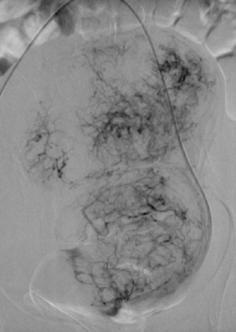
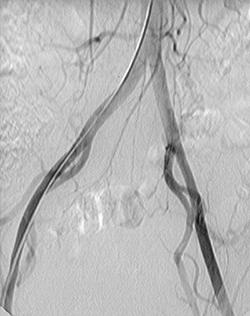
ʲôʱ������Ӧ��ע���ӹ������ѳ�������Ѫ�أ� √ ��ǰ���й���ǻ��������Ļ��� - �ӹ������г��� - �ʹ��� √ ���ѹ�-�ѳ����� - ���ѹ��� - ���ѹ�������� √ ��Ĺ����ӹ����� Pelage. Cardio Vasc Intervent Radiol 2003;26:227-30 √ �쳣�ӹ����� - �ӹ�����С - �ӹ�����ȱ�磨��������������ȱ�磩 - ˫���ӹ�����ȱ�磨��������������ȱ�磩 √ Ѫ����Ӱδ���ӹ�ʵ��Ⱦɫ�� ͼ��˫���ӹ�����ȱ�磬˫���ѳ��������빩Ѫ
�������ӹ�������Ӱ��ʾȱ���ӹ�ʵ����Ӱ ˨��ǰMRI
DSA��Ӱ
˨����������֢״����, MRI...
�Ҳ��ѳ��������빩Ѫ
���Σ��ѳ�������˨������
�ӹ�����˨��ǰӦ���ǻ����Ƿ����ѳ����������ӹ�������Ѫ��Σ�ա���õİ취����ǰ����MRA�������ӹ�����˨��ʱ�����ѳ��������빩Ѫ��Ӧ��������˨����֮�������ǻ����������Ӱ��������ֹͣ˨��������������Ӱ����Ϊ˨�����ѳ�������Ѫ����ʹ��ǻ����������Ӱ������������ǵ�˨���ѳ��������ܵķ��գ�Ӧ�ڴ�֮ǰ��ȡ���ߵ�֪��ͬ���顣
������ 1. Steven D. Abramowitz, BS, Gary M. Israel, MD, Shirley M. McCarthy, MD, PhD, Jeffrey S. Pollak, MD, Robert I. White, Jr, MD, and Michael G. Tal, MD Comparison of Four Embolic Materials at Uterine Artery Embolization by Using Postprocedural MR Imaging Enhancement. February 2009 Radiology, 250, 482-487. 2. Pelage JP, Walker WJ, Le Dref O, Rymer R. Ovarian artery: angiographic appearance, embolization and relevance to uterine fibroid embolization. Cardiovasc Intervent Radiol. 2003 May-Jun;26(3):227-33. 3. Payne JF, Robboy SJ, Haney AF. Embolic microspheres within ovarian arterial vasculature after uterine artery embolization. Obstet Gynecol. 2002 Nov;100(5 Pt 1):883-6. 4. Walker WJ, Pelage JP. Uterine artery embolisation for symptomatic fibroids: clinical results in 400 women with imaging follow up. BJOG. 2002 Nov;109(11):1262-72. 5. Abbara S, Nikolic B, Pelage JP, Banovac F, Spies JB. Frequency and extent of uterine perfusion via ovarian arteries observed during uterine artery embolization for leiomyomas. AJR Am J Roentgenol. 2007 Jun;188(6):1558-63. 6. Kim HS, Tsai J, Patra A, Lee JM, Griffith JG, Wallach EE. Effects of utero-ovarian anastomoses on clinical outcomes and repeat intervention rates after uterine artery embolization. J Vasc Interv Radiol. 2006 May;17(5):783-9. 8.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||