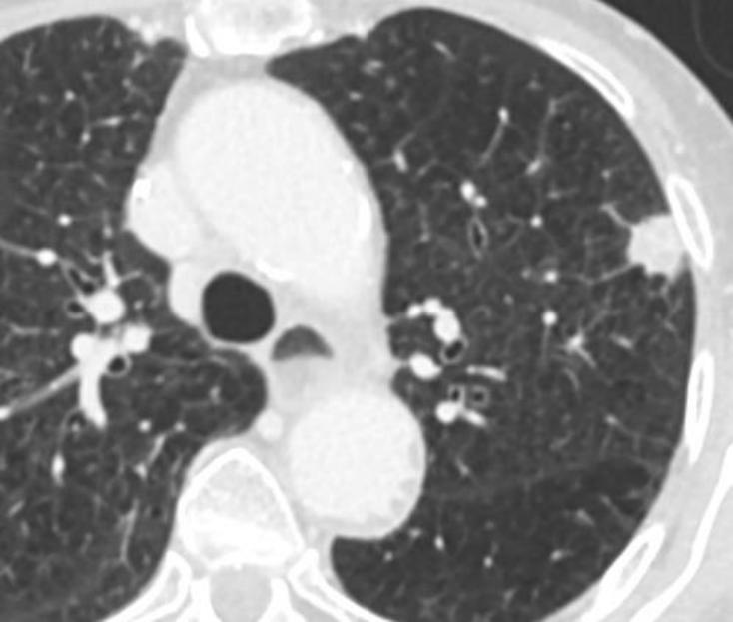
并不是只要针足够长,任何部位都可以穿刺。这种穿刺受到很多因素的限制。其可行性受到病变位置,靶病变的大小,均匀性(没有坏死腔)限制,也受到患者耐受(保持静止的能力),肺功能,凝血障碍等诸多因素限制。
|
 |
肺功能限制 Pulmonary Function Limitations
- 肺动脉高压 ( 在CT上或更好地由Swan-Ganz压力读数确定 ) Pulmonary hypertension (as determined on CT or better by Swan-Ganz pressure readings)
- 正压通气可能导致气胸或加重支气管静脉瘘并导致空气栓塞 Positive pressure ventilation may lead to pneumothorax or aggravate a bronchovenous fistula and lead to air embolism
- 严重的肺大疱性肺气肿 Severe bullous emphysema
- 对侧肺切除 Contralateral pneumonectomy
- 囊棘球蚴 Hydatid cyst
- 复发性咳嗽(咳嗽应处方)Recurrent cough (cough suppressants should be prescribed)
不能从活检中获益
有些患者因为全身状态不能接受任何治疗的情况下活检是没有意义的。有些个人可能会因为经济的问题或信仰不接受任何治疗的情况下活检也是没有意义的。
镇静剂 禁忌症 Contraindications to Sedation
Determination of periprocedural anesthesia risk is institution dependent.
围手术期麻醉风险的确定取决于机构。大型医疗机构麻醉风险较低
Many hospitals require physicians to assess the patient using the American Society of Anesthesiology (ASA) Physical Classification System and a Mallampati score.
许多医院要求医生使用美国麻醉学协会(ASA)分类系统和马兰帕蒂评分对患者进行评估。
美国医师协会⿇醉ASA分级:
美国医师协会⿇醉ASA分级:
| Ⅰ级 | 体格健康,发育营养良好,各器官功能正常。围手术期死亡率0.06%-0.08%; |
| Ⅱ级 |
除外科疾病外,有轻度并存病,功能代偿健全。围手术期死亡率0.27%-0.40%;
|
| Ⅲ级 |
并存病情严重,体力活动受限,但尚能应付日常活动。围手术期死亡率1.82%-4.30%;
|
| Ⅳ级 | 并存病严重,丧失日常活动能力,经常面临生命威胁。围手术期死亡率7.80%-23.0%; |
| Ⅴ级 | 无论手术与否,生命难以维持24小时的濒死病人。围手术期死亡率9.40%-50.7%; |
| VI级 | 确证为脑死亡,其器官拟用于器官移植手术。 |
一、二级病人麻醉和手术耐受力良好,麻醉经过平稳。三级病人麻醉有一定危险,麻醉前准备要充分,对麻醉期间可能发生的并发症要采取有效措施,积极预防。四级病人麻醉危险性极大,即使术前准备充分,围手术期死亡率仍很高。五级为濒死病人,麻醉和手术都异常危险,不宜行择期手术。
The ASA in 2014 provided greater detail to the classification regarding what constitutes a threat to life .
2014年的ASA提供了关于什么构成生命威胁的更详细的分类(主要是第4类或第三类)。
Symptomatic CHF, sepsis, and myocardial infarction or stroke within 3 months constitute class 4 disease.
3个月内有症状的慢性心功能不全、脓毒症、心肌梗死或中风构成第4类疾病。
In general, an uncontrolled or worsening neurologic, respiratory, cardiac, hematologic, or renal situation can qualify as a threat to life.
一般来说,不受控制或恶化的神经系统、呼吸、心脏、血液或肾脏情况可能成为对生命的威胁。
If the patient is ASA class 4 or higher, has unstable risk factors not qualifying as ASA class 4, and/or has any other anesthetic risk factors (such as a "difficult" airway), then some institutions and authors recommend or even require that the patient should have anesthesiology and/or other clinical subspecialist consultation prior even to otherwise "low risk" sedation procedures (Cohn S, ed.
如果患者是ASA4级或更高,有不稳定的ASA4级的危险因素,并且/或有任何其他麻醉危险因素(如气道“困难”),一些机构和文献作者要求在麻醉学和/或其他临床亚专家,甚至患者在低风险镇静操作前会诊
This consultation is to determine whether the risk factor is modifiable/able to be made stable and/or whether extra help should be available during the procedure.
会诊是为了确定风险因素是否可改变/能够使其保持稳定,以及/或在手术操作过程中是否应提供额外的帮助。
It is suboptimal patient care for the radiologist to discover risk factors the day of the procedure and/or to proceed with the biopsy out of the desire to "just get it over with.
对于介入放射科医生来说,在手术当天发现患者有风险因素和/或继续进行活检不是理想的选择。
" Patients with difficult airways or low threshold for sequelae of pneumothorax may need to have extra equipment and medications available in the room and/or healthcare personnel made available prior to the procedure to assist with complications.
困难气道或气胸后遗症阈值低的患者可能在手术前需要额外的设备和药物和/或医疗人员,以协助治疗并发症。
出血风险
SIR "standards of practice" recommendations for the cessation of antiplatelet and anticoagulant medications for interventional radiology procedures are categorized based on hemorrhage risks from level 1 to level 3.
美国“实践标准” 推荐介入放射学操作停止抗血小板和抗凝药物的建议根据出血风险从1级至3级进行分类。【Part I:Davidson 2019】【Part II :Patel 2019】
Percutaneous lung lesion biopsy is classified as a level 2 procedure. For such procedures, the SIR recommends an INR of no more than 1.5 and a platelet count of at least 50,000 cells/microliter.
Percutaneous lung lesion biopsy is classified as a level 2 procedure. For such procedures, the SIR recommends an INR of no more than 1.5 and a platelet count of at least 50,000 cells/microliter.
经皮肺病变活检分为2级手术。对于此类程序,SIR建议的INR不超过1.5,血小板计数至少为5万个细胞/微升。
The same guidelines offer specific criteria for the cessation of antiplatelet and anticoagulant medications for level 2 procedures.
同样的指南为二级手术的抗血小板和抗凝药物提供了停止的具体标准【Patel 2013】。
In the Johns Hopkins Surgical Risk Classification System, which is based primarily on the potential need for blood replacement, percutaneous lung lesion biopsy is considered to be a category 2 procedure (blood loss up to 500 cc) on a scale of 1-4.
在约翰霍普金斯外科风险分类系统中,主要基于血液置换的潜在需求,经皮肺病变活检被认为是第2类手术(失血量高达500cc),规模为1-4。
This is equivalent in risk to laparoscopic cholecystectomy and inguinal hernia repair.
这与腹腔镜胆囊切除术和腹股沟疝修补术的风险相当。
Both of these procedures are almost always performed with the aid of an anesthesiologist or certified registered nurse anesthetist present who can help with hemodynamic correction, as well as with airway maintenance and analgesia.
这两种手术几乎都在麻醉师或注册麻醉师的帮助下进行,他们可以帮助血流动力学纠正,以及气道维护和镇痛。
A rapid large pneumothorax can cause a degree of chest pain similar to that of a heart attack or aortic dissection.
快速的大气胸可引起一定程度的胸痛,类似于心脏病发作或主动脉夹层。
Some lesions can be anticipated to be highly vascular, such as a renal cell carcinoma or melanoma metastasis.
一些病变可以预期是高血管性的,如肾细胞癌或黑色素瘤转移。
It may be that there is no more reasonable alternative than percutaneous lung lesion biopsy for the next step in a patient's management despite one of the above contraindications.
尽管有上述禁忌症之一,但在患者的下一步治疗中,可能没有比经皮肺病变活检更合理的选择了。
A patient may have poor cardiopulmonary function that would be more likely to lead to death during surgery than during pneumothorax, pulmonary hemorrhage, or other complication from lung biopsy.
患者的心肺功能较差,在气胸、肺出血或其他肺活检并发症时更有可能导致死亡。
Or the diagnosis of cancer may be considered too tenuous in the mind of the oncologist that treatment with radiation or chemotherapy would be considered unacceptable without tissue confirmation.
或者,肿瘤学家可能认为癌症的诊断过于脆弱,因为如果没有组织确认,放疗或化疗将被认为是不可接受的。
In these circumstances, as suggested by the language of the NCCN and ACCP guidelines, it is the responsibility of a team of physicians (primary care, oncology, surgery, pulmonology, etc. to work together to optimize the patient ( respiratory function, blood pressure, glucose level, coagulation ability), to be ready to assist immediately for percutaneous lung lesion biopsy complications, and to set expectations for the patient.
在这种情况下,根据NCCN和ACCP指南的建议,这是一个医生团队的责任(家庭医生、肿瘤学、外科、呼吸内科或胸外科共同努力,以优化患者(包括呼吸功能、血压、血糖水平、凝血能力等),做好立即协助处理经皮肺病变活检并发症的,并为患者设定期望,告知肺活检可能出现的并发症高于通常。
其它可能风险 Other
The reality of percutaneous lung lesion biopsy is that it is often performed on highly mobile targets without the use of real-time imaging guidance.
经皮肺病变活检的现实是,它通常是在高度移动的靶病变上进行的,而不是实时影像引导。
In this setting, a "noncooperative" patient (i.e.a person who cannot lie still or breathe in a controlled fashion for the time needed to perform the biopsy) is a major contraindication to continuing with the procedure.
在这种情况下,一个非合作的病人(i.e.不能静止躺下或控制呼吸进行活检所需的时间)是继续活检的主要禁忌症【Lai 2012】。
Cooperation is usually a modifiable risk factor (discussed in brief below). 合作通常是一个可修改的风险因素(下文将简要讨论)。
Pretreatment histopathology: always?
 |
|
In the setting of a resectable and highly suspicious lesion for lung cancer, preoperative biopsy maybe unnecessary
|
肺活检禁忌症 Contraindications?!
1) 不能纠正的凝血障碍 Significant coagulopathy that cannot be adequately corrected
2) 严重的呼吸功能不全(最大呼气容积<35%) Severe respiratory insufficiency (FEV<35%)
3) 肺动脉高压>50mmHg(Pulmonary hypertension > 50 mmHg)
4) 肺气肿晚期 Advanced pulmonary Emphysema
5) 无安全的穿刺路径 Lack of safe pathway to the lesion
6) 活检位置不能或不配合 Inability of the patient to cooperate/ be positioned for the procedure
7)可切除的,高度怀疑肺癌的术前活检是不必要的
 |
可切除性和高可疑病变为肺癌,术前活检可能不必要
1. 切除后的临时检查
2. 最佳治疗(肺叶切除&淋巴结清扫)
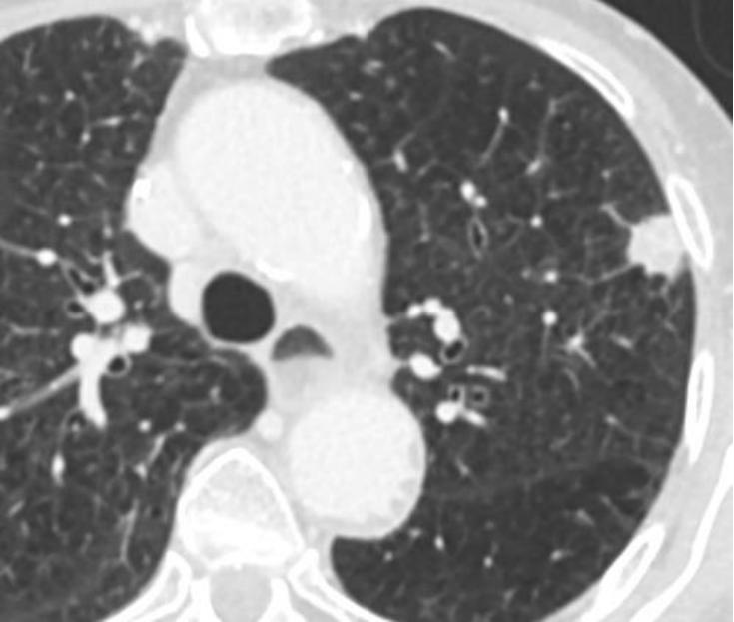
PET/CT 有助于肺结节的处理:减少不必要的穿刺
 |
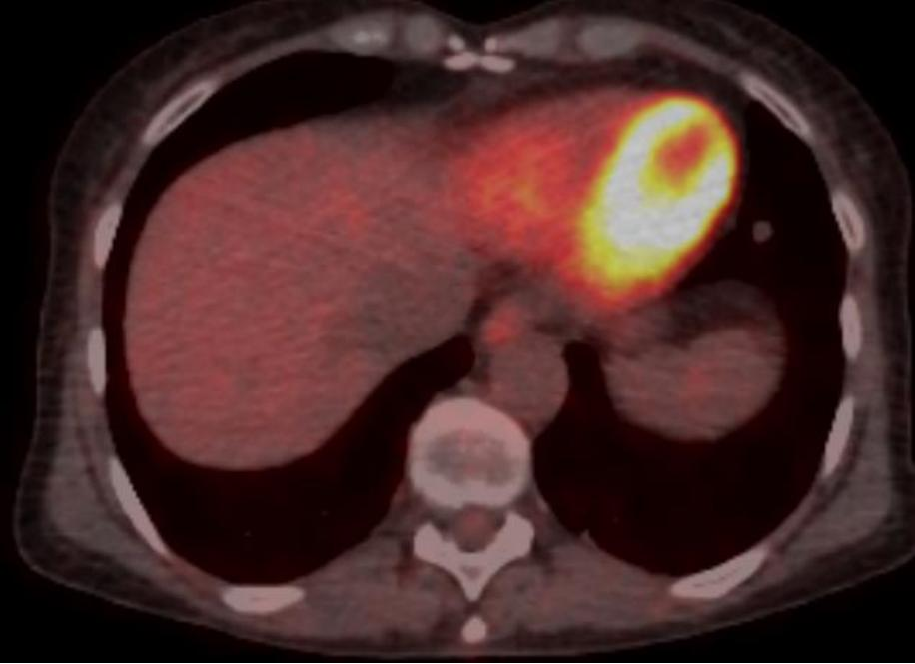 |
| patient with newly diagnosed uterine cervical cancer → curative tx |
没有代谢的孤立性肺结节:Reduce the need of puncture of non-enhancing solid nodules > 1 cm
|
绝对的禁忌症
没有知情同意书签字
不能控制的凝血功能障碍
肺血管病变
相对禁忌症
o 多学科讨论和伦理委员会评估的患者 MDT discussion and B/R evaluation
o 肺功能不好 Altered lung function (FEV1 < 35%)
o 其它凝血障碍 Other coagulopathies
o 肺动脉高压 PAH
o 一个(单个)肺的患者 Single lung patient
o 不合作患者 Uncooperative patient 在任何情况下 患者都必须配合,因为他们需要在手术和恢复期限制活动。
: