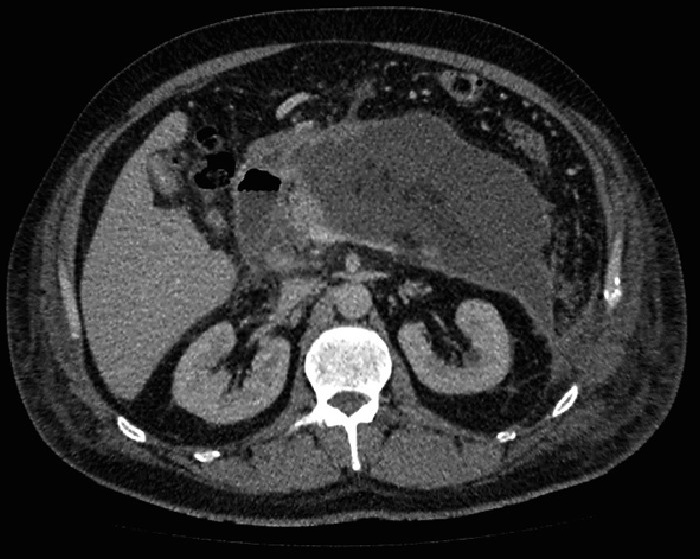
急性坏死性胰腺炎的周围积液(Collections associated with Acute Pancreatitis)包括: 1. 急性胰腺炎周围积液(Acute Peripancreatic Fluid Collection) 2. 急性胰腺脓肿(Acute Pancreatic Abscess) 3. 急性胰腺炎囊肿(Acute Pseudocyst) 另一种更为具体的分类
与经皮引流有关的SAP局部并发症的演变
急性液体的积聚 • 发生大约40%的病例(Occur in 40% of cases of Acute Pancreatitis)
• 主要在胰腺周围(Located near pancreas)
• 没有肉芽组织形成的壁(Lack a wall of granulation tissue)
• 最初通常是无菌的(Usually sterile initially)
• 持续4~6周(Persist 4-6 weeks)
• 50% 的自发性回归(regress spontaneously)
目前国际上公认的临床实践是保守治疗( Current internationally accepted clinical practice is for conservative management),这些治疗的适应症包括:(Indications to treat can include)
• 感染(Infection)
• 疼痛(Pain)
• 液体聚积不断增加(Increasing size)
• 胆道梗阻(Biliary obstruction)
引流急性胰腺炎的无菌性液体积聚有证据吗?(Draining sterile fluid collections in Acute Pancreatitis. Any evidence?)
• 随机试验(Randomised study)的研究发表在 (Surg Endosc 2011,Zerem et al)
作者结论:导管治疗比保守治疗更有效
但是B组20例病人中的11例因为导管引流发生感染,包括1例致命;so by definition ALL of Group B were de novo converted to a more aggressive management strategy
所以尽管作者有其结论,但事实上这项研究并不支持急性胰腺炎的无菌聚集液体的经皮引流
Walser较早的研究报告指出无菌聚集液体的经皮引流,感染率(contamination)为59%(CVIR 2006)
急性假性囊肿(Acute Pseudocyst)
• 富含淀粉酶的液体由纤维组织壁或肉芽组织所包裹(Collection of amylase-rich pancreatic fluid enclosed by a wall of fibrotic tissue or granulation tissue)
• 一般发生在胰腺炎发病后6周(Generally occurs 6 weeks after the acute event)
• 并非所有的假性囊肿都需要引流(Not all require drainage)
• 适应症包括(Indications include)
• 感染 Infection
• 痛疼 Pain
• 增大 Enlargement
• 胆道梗阻 Biliary obstruction
• 和主胰管的交通是重要的预后因素,因此目前推荐引流前先行ERCP(Banks et al 2011)
Communication with the Main Pancreatic Duct is an important prognostic indicator therefore current state-of-the-art recommendation is for ERCP prior to drainage (Banks et al 2011)
• 和正常主胰管有交通意味着可能延长引流的时间,但最终会成功
Communication with a normal MPD indicates likely prolonged drainage but ultimate success
• 和阻塞的主胰管交通,意味着单纯假性胰腺囊肿的引流很可能失败
Communication with an obstructed MPD indicates likely failure of catheter drainage alone
急性胰腺脓肿(Acute Pancreatic Abscess)- 最新亚特兰大(2011)共识已经取消胰腺脓肿的名词,编者认为其很难和感染坏死的液体区分。
• 邻近胰腺的边界清楚的脓液聚积(A well defined collection of pus usually adjacent to the pancreas)
• 可以包括感染性的假性胰腺囊肿(Can include infected pseudocysts)
• 通常发生在急性胰腺炎发作后3-6周(Generally occur 3-6 weeks after the acute episode)
• 与感染性胰腺坏死相区别的要点是内容物为液化,和有或没有胰腺的坏死组织
Differentiated from Infected Pancreatic Necrosis pathologically in that the contents are liquifactive and contain little or no necrotic pancreatic tissue
• 常需要长期的导管引流,如数周或数月
Often require multiple catheters over a very prolonged period ie weeks-months
• 经皮引流的成功率65-90%
胰腺坏死感染
感染的诊断(Diagnosing Infection)
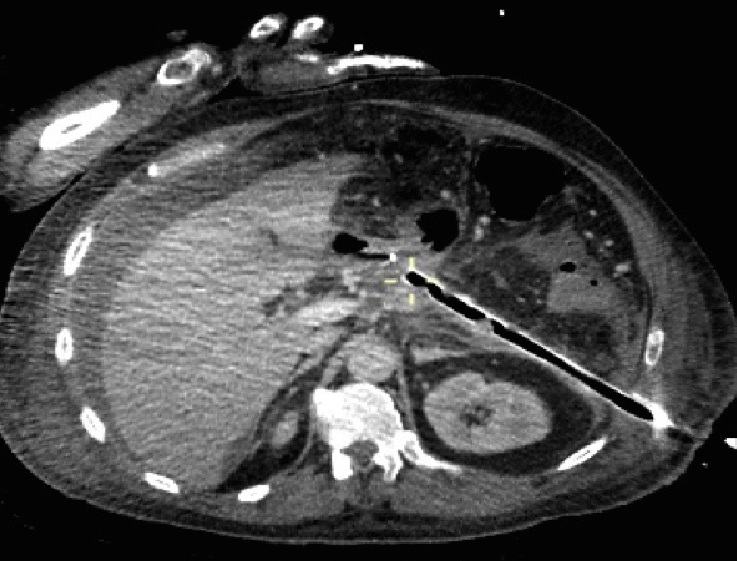
• 怀疑胰腺感染应该影像引导下抽吸因为(Suspected infection of a pancreatic collection should be dx by percutaneous image-guided aspiration as:)
• 样本错误率低(虽然有一项研究显示假阴性10%) Sampling error is low (although a false negative rate of 10% reported in one series)
• 临床和实验室感染证据,C反应蛋白和WBC 升高,发热(Clinical and Lab indicators of infection - elevated WCC, CRP, fevers - all common in Acute Pancreatitis even without infection so on their own are poor indicators)
• Multiorgan failure - suggestive but not specific nor sensitive for
infection
• No reliable imaging parameters
• 50% of patients do not present in an overtly clinically septic
manner
目标:控制感染来源,而不是完全清除坏死组织 the step-up approach aims at control of the source of infection, rather than complete removal of the infected necrotic tissue. T 第一步:经皮或内窥镜引流被感染的积液以控制败血症,这一步骤可以推迟,甚至避免外科坏死物质清除术【1-3】。 The first step is percutaneous or endoscopic drainage of the collection of infected fluid to mitigate sepsis; this step may postpone or even obviate surgical necrosectomy. 第二部:如果引流没有导致临床改善,第二部是微创腹膜后坏死组织切除【 If drainage does not lead to clinical improvement, the next step is minimally invasive retroperitoneal necrosectomy. The step-up approach may reduce the rates of complications and death by minimizing surgical trauma (i.e., tissue damage and a systemic proinflammatory response) in already critically ill patients. 粗管
多管 1. Freeny PC, Hauptmann E, Althaus SJ, Traverso LW, Sinanan M. Percutaneous CT-guided catheter drainage of infected acute necrotizing pancreatitis: techniques and results. AJR Am J Roentgenol 1998;170:969-975 2. Baril NB, Ralls PW, Wren SM, et al. Does an infected peripancreatic fluid collection or abscess mandate operation? Ann Surg 2000;231:361-367 3. Papachristou GI, Takahashi N, Chahal P, Sarr MG, Baron TH. Peroral endoscopic drainage/debridement of walled-off pancreatic necrosis. Ann Surg 2007;245:943-951 |