如何进行肱动脉穿刺?How to perform brachial arterial puncture?
历史:
第一次描述肱动脉穿刺进行血管造影的文章发表在1963年。The first paper which describes a brachial artery puncture to perform angiography published in 1963。
Bruns Beitr Klin Chir. 1963 Dec;207:398-403
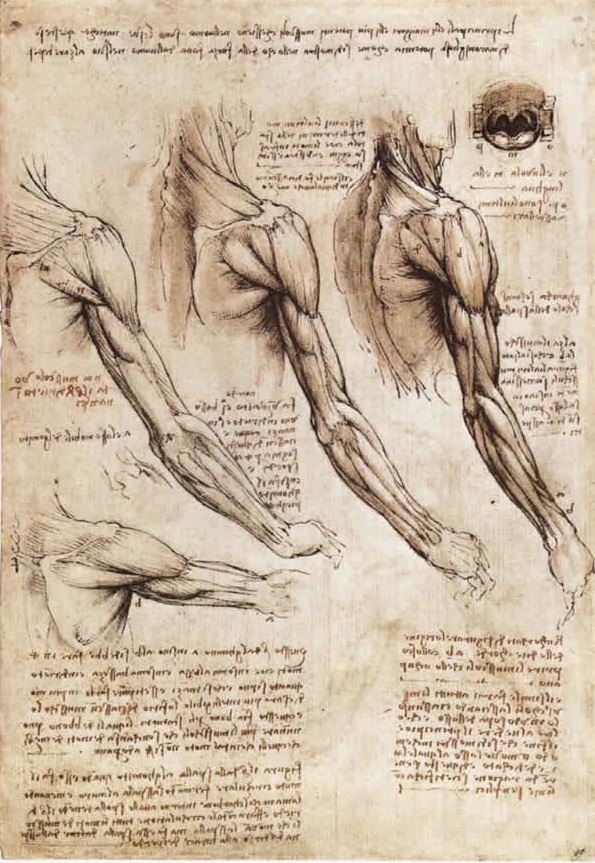
解剖:
腋动脉延续超出大圆肌下缘 (In continuation of the axillary artery beyond the lower margin of teres major muscle)
上肢腹侧表面到到肘部的肘窝(Ventral surface of the arm to the cubital fossa at the elbow)
分为桡动脉和尺动脉(Divides into the radial and ulnar arteries)
肱动脉与正中神经密切相关(Brachial artery is closely related with the median nerve)
适应症:
1. 用于避免腹股沟部位穿刺的绝大多数情况(Used in the majority of cases to avoid groin puncture)
2. 股动脉无搏动(Absent femoral pulses)
3. 最近进行过穿刺部位的外科手术(Recent surgery)
4. 评价上肢动脉或动静脉瘘(Evaluate upper limb arteries or AVF)
5. 复杂覆膜支撑架(Complex endografts)
6. 有利的肾、肠系膜上动脉、腹腔动脉解剖(降主动脉)(Renal, SMA, coeliac in favorable anatomy,descending arteries)
7. 门诊病人诊断性血管造影(Diagnostic angiography in outpatients)
禁忌症:
1. INR > 2,5
2. 解剖限制(Anatomical limitations)
3. 升主动脉弓上分支转位,如移植血管(Transposition of supraortic trunks in ascending aorta ,Ex. for endoprosthesis)

锁骨上,无名动脉过度迂曲不是经肱动脉穿刺
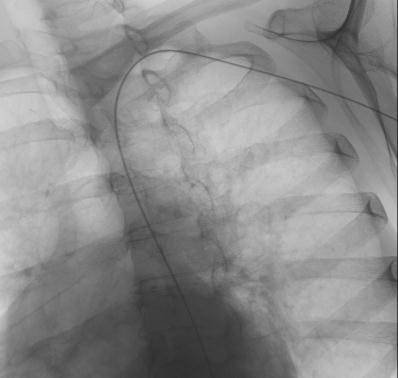
技术:
1. 2ml 2% 利多卡因局部麻醉(2cc chloridrate lydocaine 2%)
2. 经超声探头引导或直接穿刺(Linear US probe or direct puncture)
 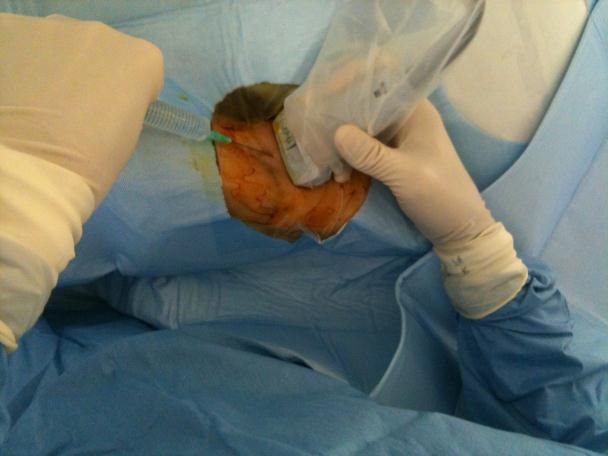 
4. 穿刺成功后,微导丝0,025’’ ~或0,035’’ 导丝经穿刺针进入血管
 
5. 经导丝置入<8F的血管鞘(Introducer sheaths ≤ 8 Fr. ,10 ~90 cm)
6. 鸡尾疗法减少血管痉挛 (Inject a pharmacological cocktail to reduce the vessel spasm)【1】
7. 将导管送入降主动脉
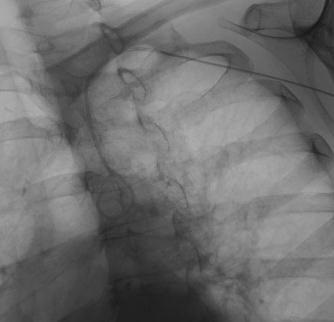 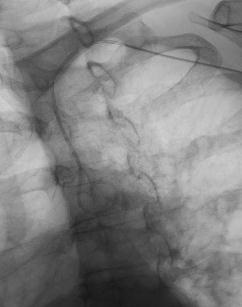 
-
用猪尾巴导管并旋转进入降主动脉(use a pigtail and rotate it to the descending aorta)
-
向下推送亲水导丝(Push down an hydrophilic guide wire)
-
随后导丝进入降主动脉(Follow the guide wire in the descending aorta)
8. 肱动脉顺行穿刺
主要应用于前臂病变的介入治疗,如手的严重或急性缺血等。
风险【3-5】:
-
抗血小板治疗减少血栓形成的风险,不增加严重出血的风险(p=0.015)(Anti platelet therapy decreases the thrombosis risks without increasing risk of significant bleeding (P = 0,015)
-
抗Vit K治疗病人有增加并发症的风险( Patients with anti Vit K treatment have an increased risk complications (P = 0,086)
-
女性风险较高,肱动脉相对细(Women have higher risks - smaller brachial arteries)
-
有经验者应用右侧肱动脉提示并不增加脑血管并发症(Several experienced groups using the right brachial artery suggested there is not an increased risk of cerebrovasc complications)
并发症
-
报告中的并发症发生率为0.9-10%(Reported 0,9 -> 10%)
-
急性血栓形成发生率(1-6%),女性较多见(Acute thrombosis ,1 – 6 % > woman)
-
夹层 0.05%(Dissections ,0,05%)
-
假性动脉瘤,0.05-0.5%(Pseudo aneurysms,0,05 – 0,5 %)
-
动脉痉挛(Arterial spasm)
-
末梢栓塞(Distal embolism ,0,04%)
-
暂短性脑缺血发作/中风(TIA / Stroke ,0,01%)
经肱动脉入路 BA ACCESS

Between January 1, 2003 and December 31, 2017, BA access was used in 157 cases performed on 136 patients. The procedures included 102 (65%) therapeutic interventions and 55 (35%) diagnostic studies. The vessels studied or treated included lower extremity arteries (48), the aorta and iliac arteries (45), mesenteric arteries (45), failing arterial revascularizations (24), renal arteries (9), subclavian arteries (8), carotid arteries (2), and visceral aneurysms (2), or in conjunction with endovascular aneurysm repair (EVAR), fenestrated EVAR, or thoracic EVAR (8). More than 1 vessel was studied or treated in 34 cases. Sheath sizes included 5F in 38 (24%) cases, 6F in 93 (59%) cases, and 7F in 26 (17%) cases. Percutaneous puncture was utilized in 142 (90.4%) cases and planned surgical exposure with primary closure of the BA in 15 (9.6%) cases (10, 7F; 4, 6F; 1, 5F). Manual compression was used for hemostasis at the conclusion of all percutaneous cases.
• BA access in 157 cases/136 patients.
• 102 therapeutic/55 diagnostic.
• Sheaths: 5F (24%); 6F (59%); 7F (17%).
• Percutaneous: 90,4%.
• Manual compression
• Access site complications 10,6% [15/142] of percutaneous access cases.
• Open surgical repair for bleeding (8) and thrombosis (7).
1. Caputo et al. Transradial Arterial Access for Coronary and Peripheral Procedures: Executive Summary by the Transradial Committee of the SCAI. Cath Cardiovasc Int 78:823–839 (2011)
2. Roberto Gandini, Georgios Angelopoulos et al. Percutaneous transluminal angioplasty for treatment of critical hand ischemia with a novel endovascular approach: “The radial to ulnar artery loop technique”; J Vasc Surg. 2010 Mar;51(3):760-2
3. Chatziioannou et al. Complications of lower-extremity outpatient arteriogra- phy via low brachial artery. Cardiovasc Intervent Radiol 2004;27: 31-34.
4. Tavris et al. Risk of local adverse events following cardiac catheterization by hemostatic device use and gender. Invasive Cardiol 2004;16:459-64.
5. Gritter et al. Complications of outpatient transbrachial intraarterial digital subtraction angiography. Radiology 1987;162:125-7.
6. Heenan SD, Grubnic S, Buckenham TM, Belli AM. Transbrachial arteriography: indications and complications. Clin Radiol. 1996 Mar;51(3):205-9.
7. Kresowik et al. A prospective study of the inci- dence and natural history of femoral vascular complications PTCA. J Vasc Surg 1991;13:328-336.
8. Rath et al. Duplex ultrasound risk stratification of percutaneous puncture of the brachial artery for diagnostic and interventional coronary angiography. Z Kardiol 1998;87:249-257.
|
