| 结肠癌辅助化学治疗 一、全身治疗 是指结肠癌切除术(或放疗)后进行化学治疗,目的是消灭残存的病灶或亚临床病灶。但结肠癌切除术后的辅助化疗同时意味着结肠癌肝转移的预防治疗。结肠癌肝转移的辅助治疗应该是肝转移病变切除术后的化学治疗。 过去有关结肠癌辅助治疗标准治疗是经静脉化疗氟尿嘧啶+甲酰四氢叶酸;奥沙利铂改善了转移性结肠癌病人的这种联合治疗。Andre 等人【3】联合奥沙利铂和氟尿嘧啶与单独应用氟尿嘧啶比较 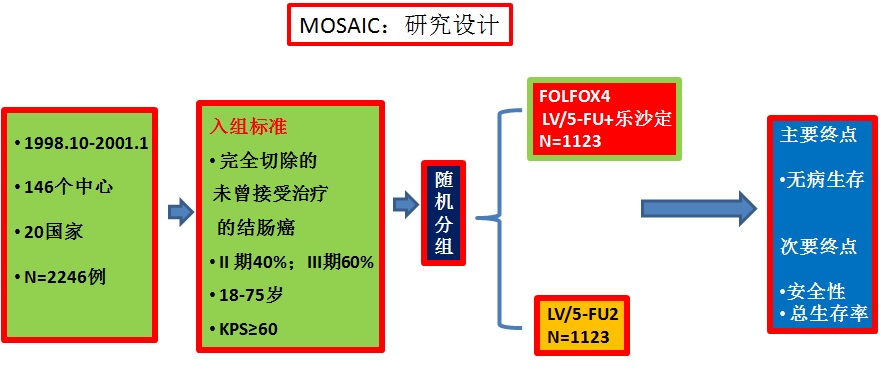 MOSAIC-COLON Adjuvant: FOLFOX vs FU/LV
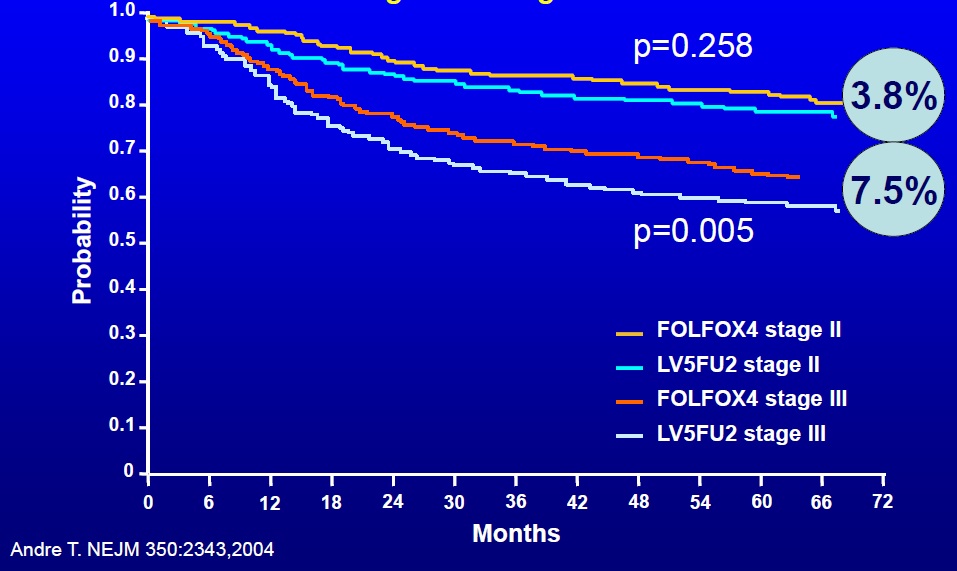
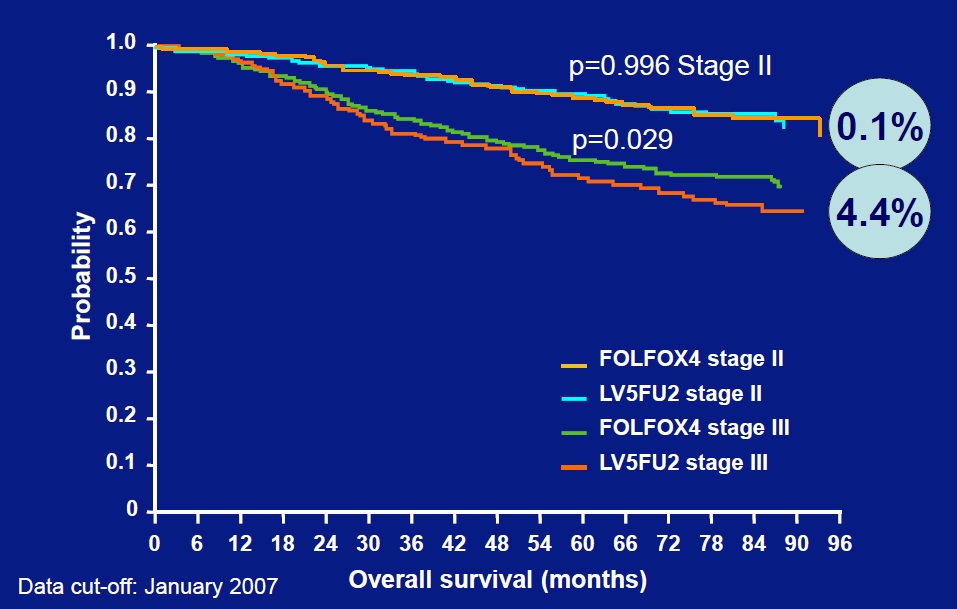
奥沙利铂是第三代铂类抗癌药。 它与5-FU/LV联合组成的FOLFOX系列方 案(L-OHP+de Gramont方案)治疗晚期 大肠癌疗效确切,耐受性好也推动了采 用FOLFOX方案作为大肠癌辅助化疗的有 关研究。 MOSAIC研究一项大型国际前瞻性随机Ⅲ期临床试验。N=2246例,Ⅱ期(40%)和Ⅲ期 (60%)大肠癌根治术后患者随机入组,6 个月内分别采用FOLFOX 4方案和5-FU/ LV方案辅助化疗12个周期; ESMO'2004 发表中位随访 44.2个月的结果。对所有患者而言,FOLFOX4组 的3年DFS率为77.9%,而5-FU/LV方案 组为72.8%,HR(95%CI)为0.76(0.64~ 0.89),P=O.0008,有显著的统计学意义, FOLFOX4组的复发危险下降了24%。 Ⅲ期大肠癌患者进行分析,3年DFS为 72.8 vs.65.8%, HR(95%CI)为0.75 (0.62~0.90),P=0.002,可降低25% 的复发风险。 Ⅱ期患者中,DFS为 87.4% vs.84.3%, HR(95%CI)为0.79 (0.57~1.09),P=0.151,观察 到FOLFOX 4方案降低21%的复发风险。 在安全性方面,中性粒细胞减少和血小板减少和神经毒性方面,FOLFOX4组高于5-FU/LV组,但最终两组 的治疗相关死亡率相同(0.5%)。据此, 2004年欧洲药品委员会和美国FDA分别批准 L-OHP扩大适应证,即分别允许允许其在欧盟范围内用于Ⅲ期结肠癌原发灶完全切除后的辅助治疗和L-0HP联合5-FU/LV用于原发病灶根 治术后的Ⅲ期结肠癌的辅助化疗。
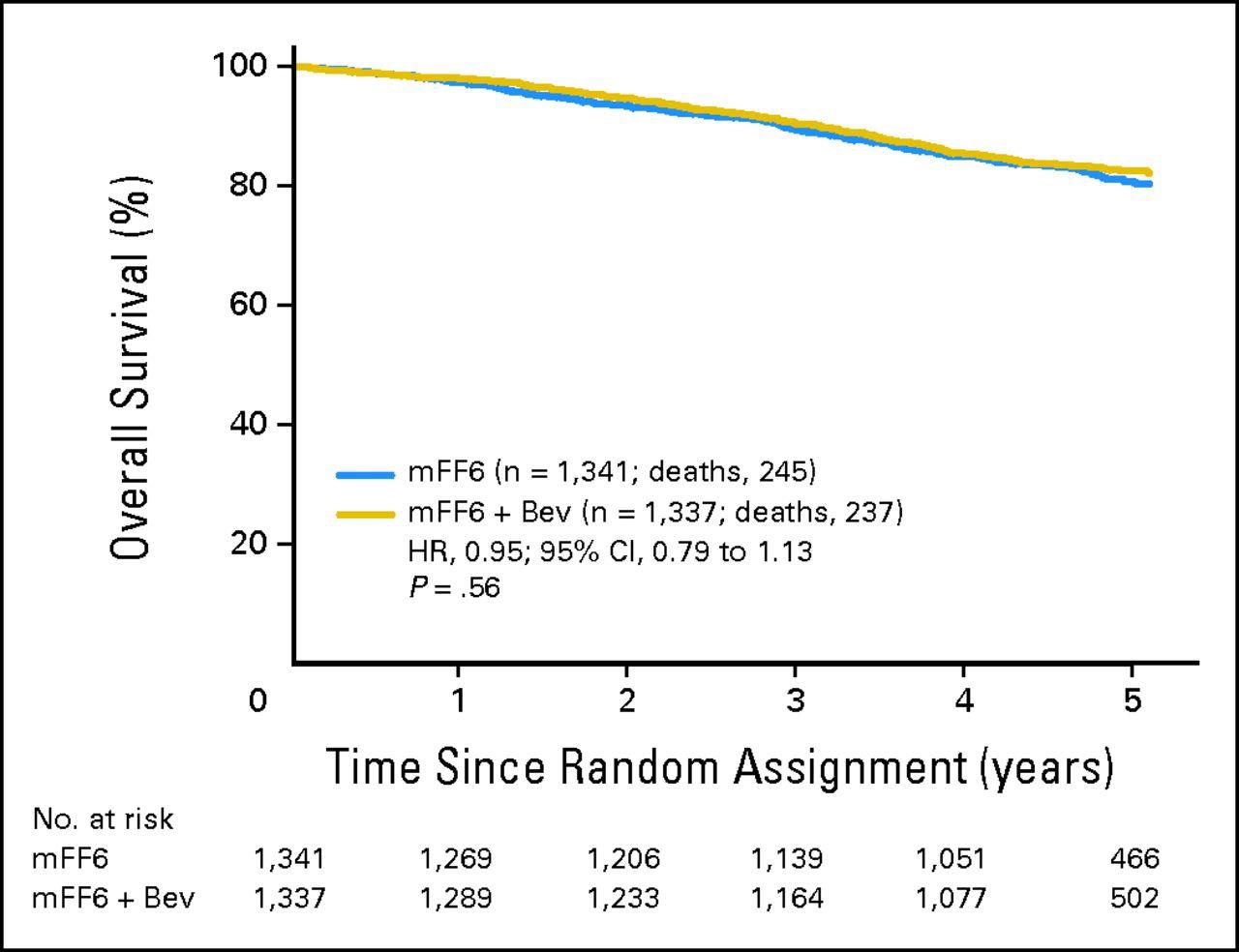
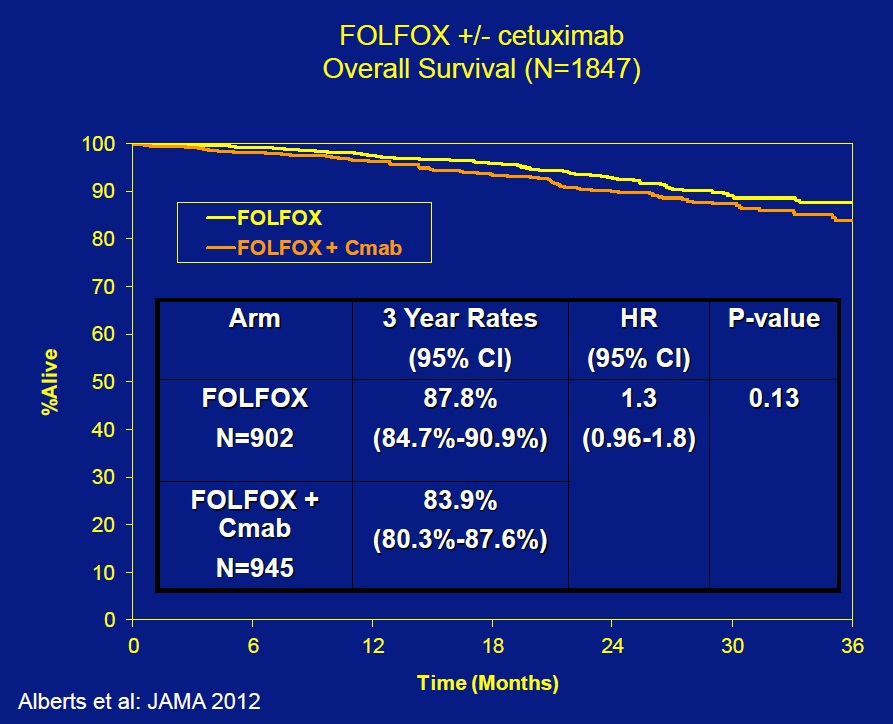
FOLFOX +/- cetuximab:Overall Survival (N=1847)
结论原发结肠癌传统辅助治疗:
二、肝转移癌肝切除后动脉灌注化疗结果 1. MSKCC 【1】
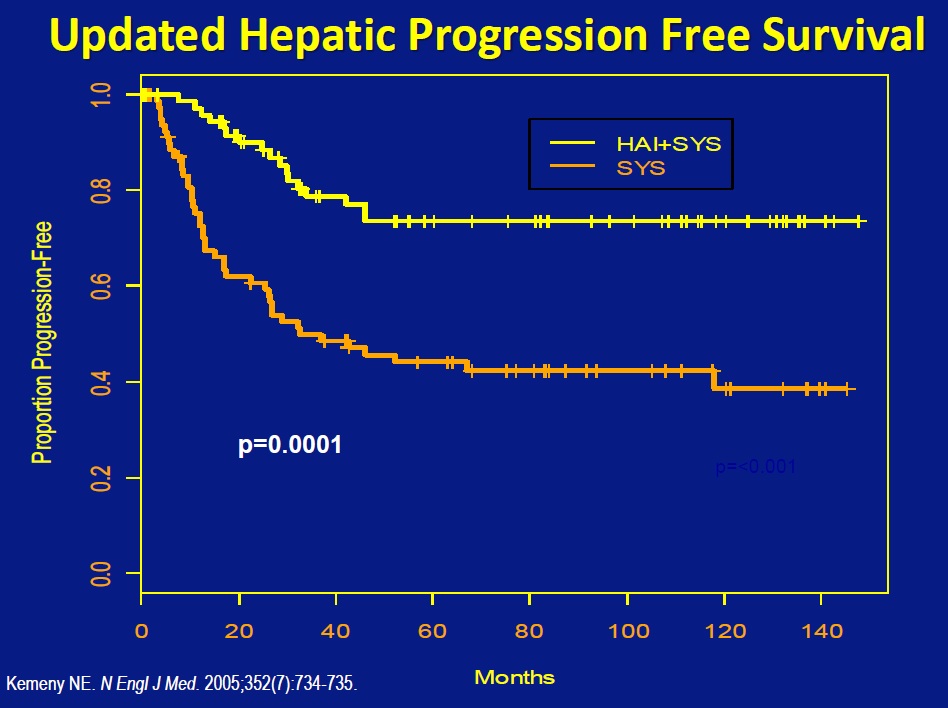
2005年纪念斯隆-凯特林癌症中心(Memorial Sloan Kettering Cancer Center,MSKCC)的Nancy E. Kemeny 发表了结肠癌不可切除肝转移肝动脉灌注+全身化疗与单独全身化疗的比较【1】。 此后Nancy 发表了一系列关于结肠癌肝转移的动脉灌注化疗的研究【2-18】。 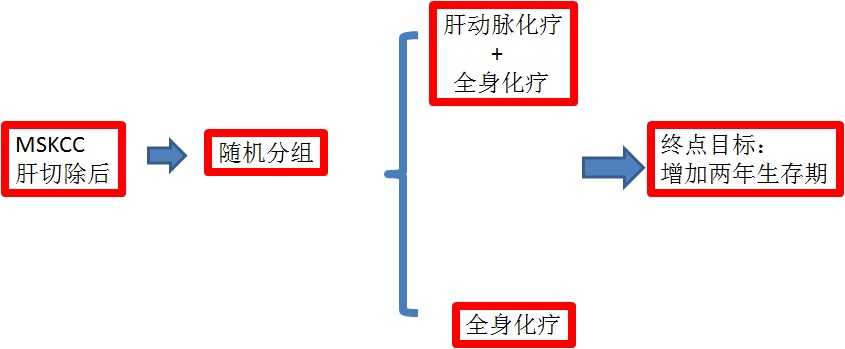 统计学方法:156例样本,增加2年生存率p=0.05显著水平,有80%的把握度。(156 pts were required to detect increase in 2-year survival with 80% power at a 5% significance level) 结果
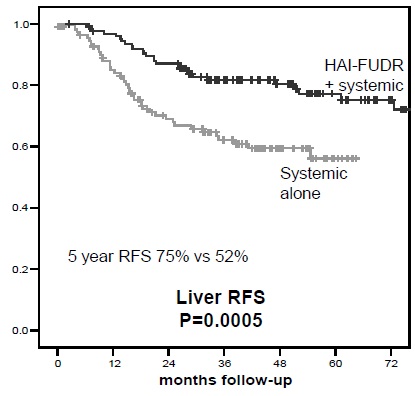
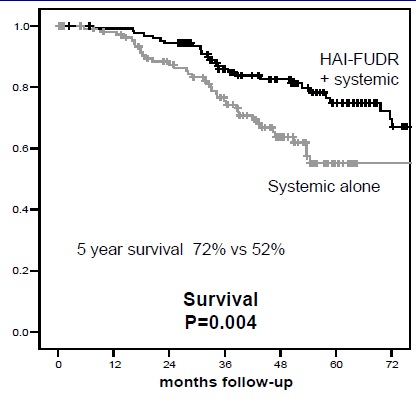
2. 包括MSKCC在内多项关于 肝切除后肝动脉灌注对全身化疗或对照研究
Randomized Studies After Liver Resection HAI vs SYS or Control:Hepatic Disease-Free Survival
Randomized Studies After Liver Resection HAI vs SYS or Control:Disease-Free Survival
3. Modern Systemic Therapy as Adjuvant Therapy after Liver Resection
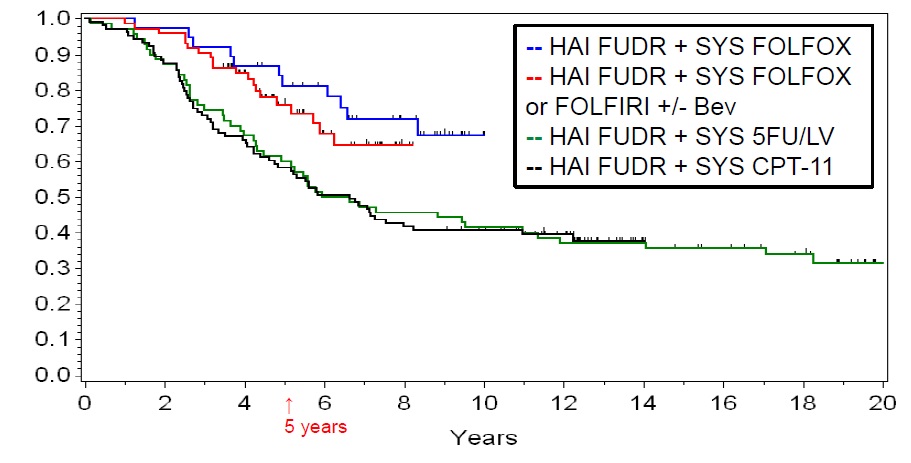
4. 化疗方案不同 HAI+ SYS- Overall Survival by Protocol
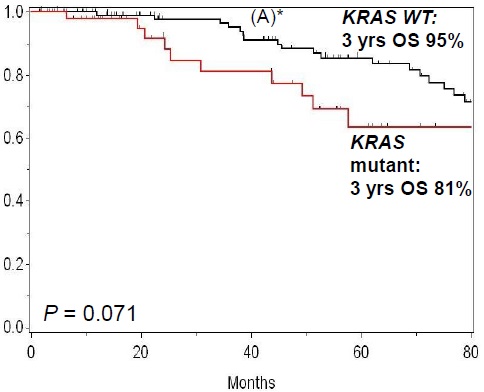
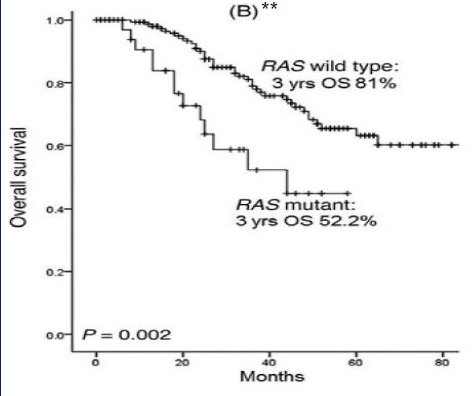
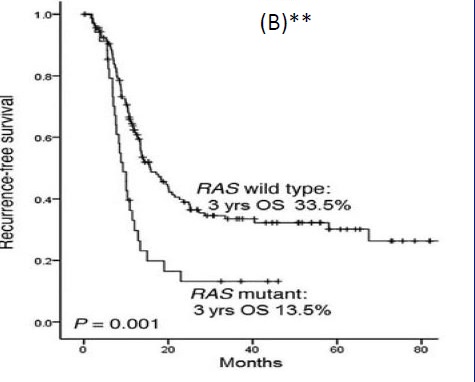
5. 以基因分类不同
*Kemeny N. J Clin Oncol 30: 2013;**Vauthey JN. Ann Surg. 2013;258(4): 619-27
1. Kemeny N, Jarnagin W, Paty P, Gönen M, Schwartz L, Morse M, Leonard G, D'Angelica M, DeMatteo R, Blumgart L, Fong Y. Phase I trial of systemic oxaliplatin combination chemotherapy with hepatic arterial infusion in patients with unresectable liver metastases from colorectal cancer. J Clin Oncol. 2005 Aug 1;23(22):4888-96. Epub 2005 Jul 11.
Recurrence Free Survival (RFS) by KRAS Liver Resected Patients
结论:肝切除术后,肝动脉灌注+静脉化疗 与单独静脉化疗随机临床试验比较显示前者显著增加结直肠癌肝转移DFS(hepatic & overall) 2. Kemeny N, Eid A, Stockman J, Gonen M, Schwartz L, Tetzlaff E, Paty P. Hepatic arterial infusion of floxuridine and dexamethasone plus high-dose Mitomycin C for patients with unresectable hepatic metastases from colorectal carcinoma. J Surg Oncol. 2005 Aug 1;91(2):97-101. 3. Kemeny NE, Niedzwiecki D, Hollis DR, Lenz HJ, Warren RS, Naughton MJ, Weeks JC, Sigurdson ER, Herndon JE 2nd, Zhang C, Mayer RJ. Hepatic arterial infusion versus systemic therapy for hepatic metastases from colorectal cancer: a randomized trial of efficacy, quality of life, and molecular markers (CALGB 9481).J Clin Oncol. 2006 Mar 20;24(9):1395-403. Epub 2006 Feb 27. 4. Kemeny N. Management of liver metastases from colorectal cancer. Oncology (Williston Park). 2006 Sep;20(10):1161-76, 1179; discussion 1179-80, 1185-6. Review. 5. Kemeny N, Brown K, Covey A, Kim T, Bhargava A, Brody L, Guilfoyle B, Haag NP, Karrasch M, Glasschroeder B, Knoll A, Getrajdman G, Kowal KJ, Jarnagin WR, Fong Y. Phase I, open-label, dose-escalating study of a genetically engineered herpes simplex virus, NV1020, in subjects with metastatic colorectal carcinoma to the liver. Hum Gene Ther. 2006 Dec;17(12):1214-24. 6. Kemeny N. Presurgical chemotherapy in patients being considered for liver resection. Oncologist. 2007 Jul;12(7):825-39. Review. 7. Kemeny N, Capanu M, D'Angelica M, Jarnagin W, Haviland D, Dematteo R, Fong Y. Phase I trial of adjuvant hepatic arterial infusion (HAI) with floxuridine (FUDR) and dexamethasone plus systemic oxaliplatin, 5-fluorouracil and leucovorin in patients with resected liver metastases from colorectal cancer. Ann Oncol. 2009 Jul;20(7):1236-41. doi: 10.1093/annonc/mdn769. Epub 2009 Feb 20. 8. Kemeny NE, Melendez FD, Capanu M, Paty PB, Fong Y, Schwartz LH, Jarnagin WR, Patel D, D'Angelica M.Conversion to resectability using hepatic artery infusion plus systemic chemotherapy for the treatment of unresectable liver metastases from colorectal carcinoma.J Clin Oncol. 2009 Jul 20;27(21):3465-71. doi: 10.1200/JCO.2008.20.1301. Epub 2009 May 26.
9. Kemeny N. Role of local liver therapy for hepatic metastases from colorectal cancer. Clin Adv Hematol Oncol. 2009 Dec;7(12):815-7. No abstract available.18. Kemeny N. Postnatal support: who cares? Pract Midwife. 2014 Jul-Aug;17(7):5.
10. Kemeny N. In defense of hepatic arterial infusion for hepatic metastases of colorectal cancer. J Natl Compr Canc Netw. 2010 May;8(5):507-9. 11. Kemeny N. The management of resectable and unresectable liver metastases from colorectal cancer. Curr Opin Oncol. 2010 Jul;22(4):364-73. doi: 10.1097/CCO.0b013e32833a6c8a. Review. 12. Kemeny NE, Jarnagin WR, Capanu M, Fong Y, Gewirtz AN, Dematteo RP, D'Angelica MI. Randomized phase II trial of adjuvant hepatic arterial infusion and systemic chemotherapy with or without bevacizumab in patients with resected hepatic metastases from colorectal cancer. J Clin Oncol. 2011 Mar 1;29(7):884-9. doi: 10.1200/JCO.2010.32.5977. Epub 2010 Dec 28. 13. Kemeny NE, Schwartz L, Gönen M, Yopp A, Gultekin D, D'Angelica MI, Fong Y, Haviland D, Gewirtz AN, Allen P, Jarnagin WR. Treating primary liver cancer with hepatic arterial infusion of floxuridine and dexamethasone: does the addition of systemic bevacizumab improve results? Oncology. 2011;80(3-4):153-9. doi: 10.1159/000324704. Epub 2011 Jun 14. 14. Kemeny NE. Changing paradigms for liver resection of colorectal metastases.Ann Surg Oncol. 2012 Sep;19(9):2773-5. 15. Kemeny NE. Combining hepatic arterial infusion and systemic therapy: radiologic versus surgical approaches. J Vasc Interv Radiol. 2012 Oct;23(10):1268. 16. Kemeny NE. Treatment of metastatic colon cancer: "the times they are A-changing". J Clin Oncol. 2013 Jun 1;31(16):1913-6.
17. Kemeny NE. The re-birth of hepatic arterial infusion for colorectal liver metastases. J Gastrointest Oncol. 2013 Jun;4(2):118-20.
18. Kemeny NE, Chou JF, Capanu M, Gewirtz AN, Cercek A, Kingham TP, Jarnagin WR, Fong YC, DeMatteo RP, Allen PJ, Shia J, Ang C, Vakiani E, D'Angelica MI KRAS mutation influences recurrence patterns in patients undergoing hepatic resection of colorectal metastases. Cancer. 2014 Aug 25.doi: 10.1002/cncr.28954. [Epub ahead of print]
19. Kemeny NE, Gonen M. Hepatic arterial infusion after liver resection. N Engl J Med. 2005 Feb 17;352(7):734-5. | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||