因为不可外科治疗的内脏动脉瘤会逐渐增大,有潜在的自发破裂的可能,其早期发现和有效治疗是需要的。经导管血管内治疗技术的并发症和死亡率对不适外科治疗的患者是低的。
内脏动脉瘤定义
 6 6
内脏动脉瘤的定义
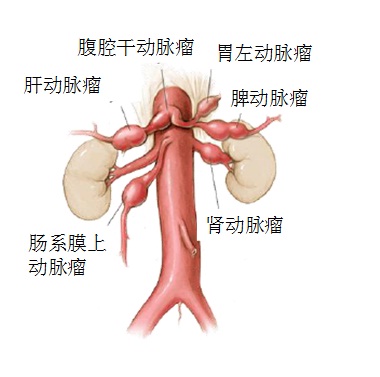
内脏动脉(Visceral Artery)包括 肝动脉,腹腔动脉,脾动脉,肠系膜上、下动脉,肾动脉等。内脏血管疾病(Vascular disease)包括 动脉狭窄,阻塞,夹层,动脉瘤和血管畸形。内脏血管疾病还包括内脏静脉血管系统疾病。
Abdominal visceral artery aneurysms (VAAs) are generally defined as aneurysms that involve branches of the celiac,superior mesenteric, inferior mesenteric, or renal arteries. 这里主要介绍内脏动脉瘤的介入治疗。
内脏动脉瘤是相对少见的血管疾病,近年来随着MRI和CT,以及血管介入治疗的开展是这类疾病偶然发现的几率升高。
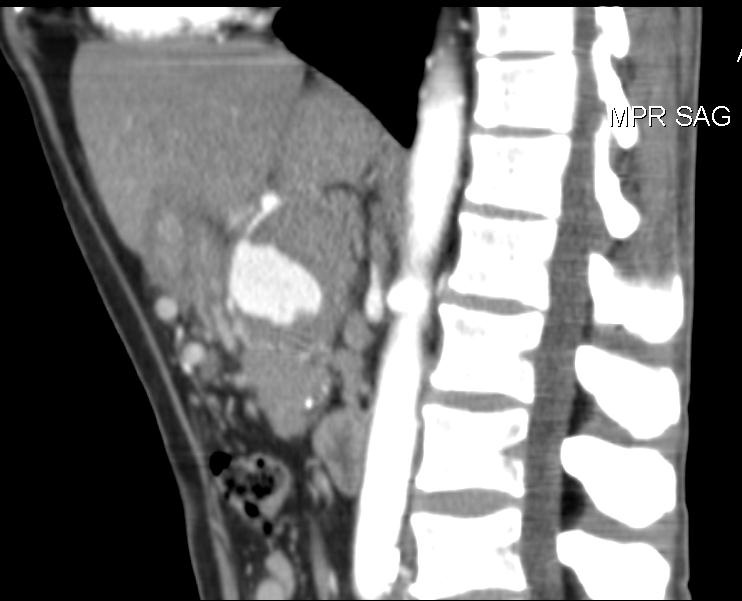
As a result of improvements in imaging technology and the increasing use of cross-sectional imaging modalities (ultrasound, computed tomography [CT], and magnetic
resonance imaging), VAAs are diagnosed with increasing frequency.
内脏动脉瘤是相对少见的血管疾病,有时偶然在尸检中发现。近年来随着MRI和CT,血管介入治疗及非血管(如胆道)的开展使这类疾病偶然发现的几率升高。人群中发病率0.1% - 2%。
(Nosher et al. Radiographics 2006;26:1687-1704 Schwartz et al. J Pathol Bacteriol. 1965;89:349-356)
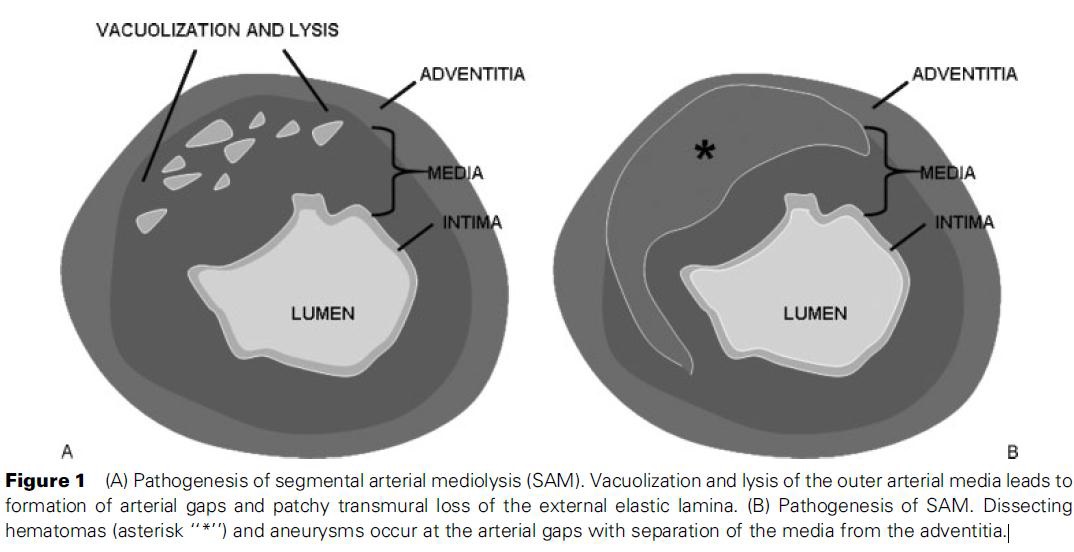
内脏动脉瘤的类型多数内脏动脉瘤继发于血管壁退变(degeneration)、动脉中层缺失和/或弹力层破碎以及平滑肌的减少。如动脉硬化性疾病,某些先天疾病,肌纤维增生不良和怀孕期间变化。而假性动脉瘤往往是钝性或穿透伤、炎症、感染、血管炎和医源性创伤(外科、内镜操作和介入治疗)
内脏动脉瘤的发病率和病因
Pasha S F et al. Mayo Clin Proc. 2007;82:472-479
肾动脉瘤
主要病因为肌纤维增生不良,动脉硬化和血管炎
Reported incidence of 0.01-0.2% on routine autopsies。报告常规尸检发生率为0.01~0.2%。
Segmental Arterial Mediolysis,SAM
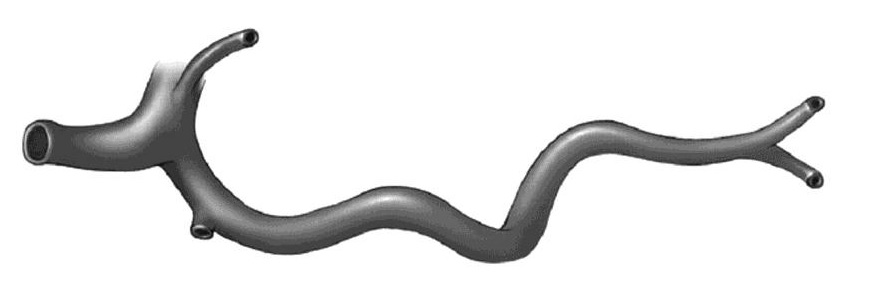
基于数个标准,内脏动脉瘤有多种分类 在病理上动脉瘤分真性动脉瘤、和假性动脉瘤;并分为各种解剖类型;多发动脉瘤或单发动脉瘤;大动脉瘤和小动脉瘤或微动脉瘤,成熟或非成熟动脉瘤。 1. 根据动脉壁的结构,分为真性动脉瘤和假性动脉瘤(病理),成熟动脉瘤或非成熟动脉瘤(内脏动脉破裂后血肿形成的腔)以及动脉瘤的解剖类型。 
A true aneurysm involves all three layers of the arterial wall. In general, a true aneurysm is defined as a localized dilatation of the artery by more than 1.5 times the expected
arterial diameter.
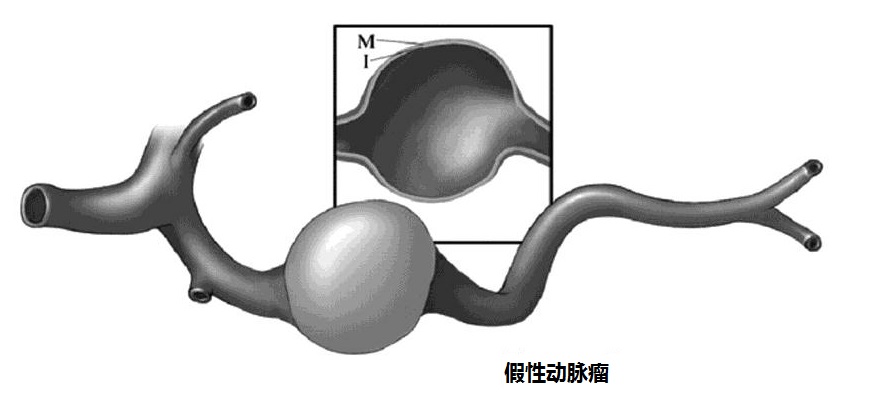
假性动脉瘤示意图
真性动脉瘤发生的潜在动脉病理包括动脉硬化,肌纤维增生不良,动脉炎。真性动脉瘤发生率0.1~2%,大部分真性动脉瘤是无症状的,少数可以引起腹痛,但这可以预示着破裂迫在眉睫。内脏动脉瘤几乎没有大到足以在体检是触摸到。
True aneurysms may occur as a result of underlying arterial pathology such as atherosclerosis, fibromuscular dysplasia, and arteritides. The prevalence of true VAAs is 0.1–2%, and most true VAAs are asymptomatic. A minority may cause abdominal pain, which may be a harbinger of imminent rupture. VAAs are almost never large enough to be palpable by examination.
假性动脉瘤
False aneurysms, or pseudoaneurysms, are effectively contained ruptures of the artery that are lined by adventitia or by the perivascular tissues. False aneurysms may occur
as a result of inflammation, infection, or trauma
2. 根据形态和结构分为囊性动脉瘤和梭形动脉瘤 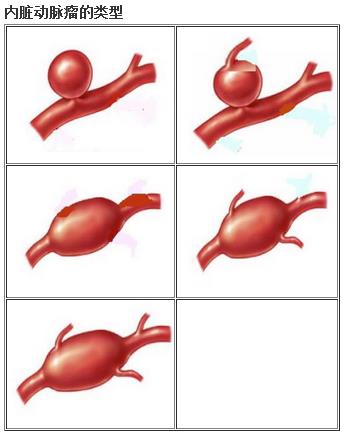 3. 根据大小分为小动脉瘤、大动脉瘤和巨大动脉瘤 4. 单发动脉瘤和多发动脉瘤 多发动脉瘤
内脏真性动脉瘤和假性动脉瘤发生的位置不一样
病理上一般将动脉瘤分为真性动脉瘤和假性动脉瘤。需要介入治疗的动脉瘤分类更细致。真性动脉瘤绝大多数发生在主干分支/分叉处。而假性动脉瘤多发生在实质器官内或胰腺周围动脉内。 内脏动脉瘤尸检发生率
据报告常规尸检内脏动脉瘤的发现率为0.01-0.2%。
内脏动脉瘤早期可以无症状 内脏动脉瘤的主要问题是早期可以完全无症状,只是由于CT及MRI检查偶尔发现。 内脏动脉瘤破裂率和死亡率 高达22%~25%在预期寿命过程中发生破裂。破裂后死亡率25%~75%(Stanley et al. J Vasc Surg 1986;3:836-840 )。22% of all VAAs present as clinical emergencies。也有人报告8.5% result in death。内脏动脉瘤破裂的因素包括大小、怀孕,肝硬化以及肝移植。 内脏动脉瘤的治疗目标 治疗的主要目标是预防破裂。破裂的主要危险因素包括动脉瘤的大小,症状性动脉瘤,如肠系膜上动脉的动脉瘤可以导致缺血。 内脏动脉瘤的治疗选择 内脏动脉瘤治疗的选择包括密切观察、外科或腹腔镜、支撑架(覆膜支撑架或多层支撑架)以及介入栓塞治疗。(Abbas et al. Ann Vasc Surg 2002;16:442-449 ; Stanley et al. J Vasc Surg 1986;3:836-840 ;Holdsworth et al. Br J Obstet Gynaecol 1992;99:595-597)
临床重要性是它潜在的致命性
传统治疗策略是基于密切观察或外科手术治疗。择期外科治疗死亡率接近5%。动脉瘤动脉瘤破裂急诊外科手术死亡率会增加【2,5】。
Traditional management strategies have been based on surveillance or surgical repair. Mortality after elective surgical repair is approximately 5%. Mortality increases substantially if emergency surgery is required for aneurysm rupture [1, 2].
外科和腹腔镜治疗治疗有较高的死亡率,破裂动脉瘤手术的死亡率为20%,而择期手术的死亡率为5%。介入治疗已经成为内脏动脉瘤首选治疗,弹簧栓子的栓塞超过对动脉瘤切除或结扎的外科手术。(Abbas et al. Ann Vasc Surg 2002;16:442-449 )
不管是内科治疗还是外科治疗分享同一目标:防止动脉瘤继续扩大和破裂。其治疗的决定是个性化,取决于位置
例如,脾动脉瘤破裂后外科死亡率为10-25%,腹腔动脉瘤破裂死亡率接近100%【1-4】。鉴于破裂动脉瘤有较高的死亡率,内脏动脉瘤超出2cm直径一般推荐择期治疗。
(2)介入治疗For example, the reported mortality rates of open surgical repair after splenic artery aneurysm rupture range from 10–25%, and approach 100% for ruptured celiac artery aneurysms [1–4]. In view of the high mortality of ruptured aneurysms, elective repair of VAAs exceeding 2 cm diameter is generally recommended.
1. Pasha SF, Gloviczki P, Stanson AW, Kamath PS (2007) Splanchnic artery aneurysms. Mayo Clin Proc 82:472–479
2. Shanley CJ, Shah NL, Messina LM (1996) Common splanchnic artery aneurysms: splenic, hepatic, and celiac. Ann Vasc Surg 10: 315–322 3. Messina LM, Shanley CJ (1997) Visceral artery aneurysms. Surg Clin North Am 77:425–442 4. Chiesa R, Astore D, Guzzo G et al (2005) Visceral artery aneurysms. Ann Vasc Surg 19:42–48 5. Huang YK, Hsieh HC, Tsai FC et al (2007) Visceral artery aneurysm: risk factor analysis and therapeutic opinion. Eur J Vasc Endovasc Surg 33:293–301 ******************************************************************************** 虽然传统治疗内脏动脉瘤的的方法是外科手术,但现代治疗策略是将介入放射治疗技术放在首位。因此,血管介入放射一声必须熟悉内脏动脉瘤介入治疗的适应症,熟练各种技术 Although classically treated by open surgery, modern treatment strategies generally place interventional radiology techniques at the top of the treatment algorithm. Therefore, vascular interventional radiologists must become familiar with the indications for the treatment of VAA, become experienced in the different techniques, and know when to recommend treatment of VAA by interventional radiology techniques or to advocate open surgical repair. In this review, we will describe the role of interventional radiology in the treatment of VAAs according to anatomy and vascular territory.
介入治疗的成功率80%~100%之间,其主要的优势包括由于微创伤手段导致的低危险,它是一项疗效十分明确的手术。可以治疗那些外科手术不能治疗的部位并不增加危险性(如肝内动脉瘤或胰腺周围的动脉瘤)。而现有技术的缺点包括,弹簧圈技术有时不得不阻断载瘤动脉;瘤囊填塞技术(或支撑架,球囊辅助技术)仅适合小动脉瘤或窄颈动脉瘤。覆膜支撑架不得不阻塞动脉瘤上的分支,并且柔顺度不够。进展中的多层支撑架技术目前的样本量还小。(– McDermott VG et al. CVIR 1994;–Abbas et al. Mayo series.Annalsof vascular surgery 2002)
内脏动脉瘤影像学的角色 Interventional radiology techniques are being used increasingly to treat VAAs, and in most centers, they are the first line of treatment. The success of interventional
radiology treatment is dependent on high-quality crosssectional preprocedural imaging and adequately trained vascular interventional radiologists.
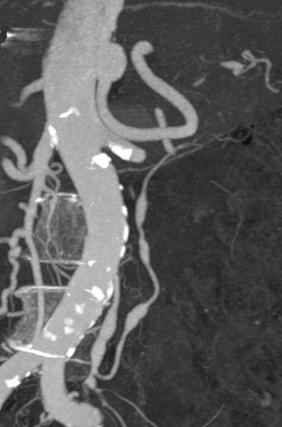
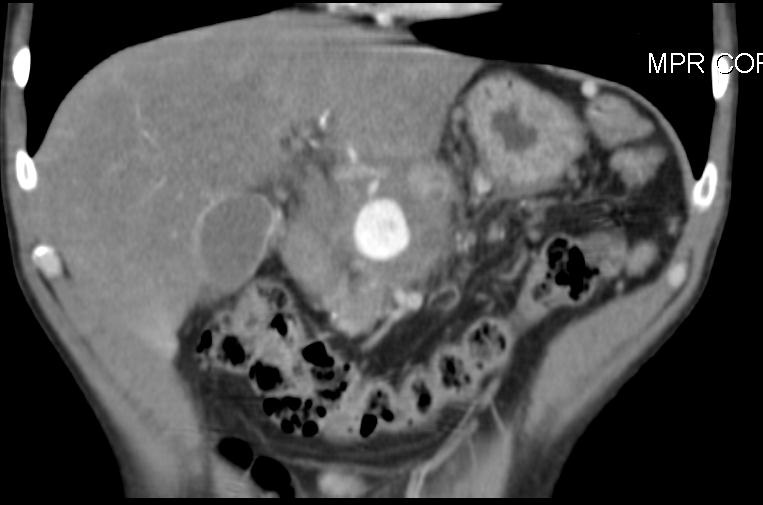
影像学检查的角色包括(1)发现病变,(2)分析病变的特征,(3)指导治疗计划的制定以及(4)随访。所有的影像学检查都扮演一定的角色。但3D-MIP、VRT-CTA为最有效的综合检查工具。这是基于对动脉瘤的位置、形态结构(body habitus)的敏感性、特异性和可重复性。避免操作复杂的DSA,为血管内治疗提供选择的目标。
Interventional radiology techniques are being used increasingly to treat VAAs, and in most centers, they are the first line of treatment. The success of interventional radiology treatment is dependent on high-quality crosssectional preprocedural imaging and adequately trained vascular interventional radiologists.
High-resolution multiplanar cross-sectional imaging answers questions concerning access vessel pathology, vessel tortuosity, suitability of a particular treatment strategy, and presence of aneurysms at other sites. Operator competence to treat VAAs requires knowledge of vascular anatomy and collateral pathways, training in the catheterization
of visceral arteries, familiarity with handling the various interventional tools, and experience in complex embolization and stenting procedures.
影像学的评估包括动脉瘤的位置、血管来源、接入/引流血管、大小、时间变化、多发性、结构(大小、形状、瘤颈特征、血栓和肿块效应)和血流。理想的影像学采集和处理还在进一步探讨中。 高质量的影像有助于发现
内脏动脉瘤的适应症
随着影像学技术的发展,内脏动脉瘤的发现增加,动脉瘤的大小被表述为主要的适应症。但目前缺乏未治疗动脉瘤的自然病史,关于干预还是监视观察的大小标准还有争论。 内脏动脉瘤的绝对适应症是症状性动脉瘤包括疼痛、出血或缺血。相对适应症包括动脉瘤>2cm 和育龄女性或孕妇。(Abbas et al. Ann Vasc Surg 2002;16:442-449 ; Stanley et al. J Vasc Surg 1986;3:836-840 ; Holdsworth et al. Br J Obstet Gynaecol 1992;99:595-597)。
The main indication for treatment is the size of the aneurysm. Because of the lack of data on the natural history of untreated aneurysms, there is debate regarding the size criteria for intervention vs. surveillance. The general consensus is that when a true aneurysm is 2 cm or larger (irrespective of anatomical site), the rupture risk is probably sufficient to indicate treatment. Aneurysms smaller than 2 cm are generally observed by serial
imaging [2, 4–7].
Other indications for treatment include symptomatic patients and documented evidence of growth of the aneurysm.In addition, most interventionalists treat smaller true
aneurysms (1–2 cm or even less) in women who wish to become pregnant; rupture of splenic artery aneurysms in pregnant women is associated with maternal and fetal
mortality [6, 8].
Whereas the decision to intervene on a true aneurysm may depend on a size threshold above which the potential for rupture increases, it is generally advised that all
pseudoaneurysms should be treated, whatever their size or location.

内脏动脉瘤治疗的适应症:有关内脏动脉瘤适应症还充满争论:动脉瘤大小、怀孕、肝硬化以及肝移植的病人有破裂危险
1. 假性动脉瘤:有人认为内脏假性动脉瘤不管大小和有无症状都需要治疗。也有认为动脉瘤<2cm,应密切影像学观察。
2. 真性动脉瘤:≥2cm,不管解剖位置,因破裂的危险足以适合干预治疗
a. 育龄非孕女性直径2.0 ~ 2.5cm的内脏动脉瘤
b. 接受肝移植病人直径2.0 ~ 2.5 cm的内脏动脉瘤
c. 症状性动脉瘤,如缺血、出血和肾血管性高血压
d. 观察随访期间动脉瘤直径增大(Documented growth of the aneurysm)
e. 肝硬化,门静脉高压 较小的真性动脉瘤(1-2cm)女性,也被考虑为干预治疗的适应症
由于对未治真性内脏动脉瘤的自然病史不清,关于动脉瘤监测或干预治疗的直径标准有争论。ACC和AHA出版指南动脉瘤治疗的直径为2.0,其它作者建议2.5cm【3,4】。钙化并不能保护动脉瘤破裂,90%动脉瘤破裂有钙化(Maher AA et al. Annals of vascular surgery 2008)
Contraindications to Treatment
Contraindications to treatment are few and can be subdivided into contraindications to surgical treatment (usually based on patient comorbidity) and contraindications
to interventional radiology.
Relative contraindications to interventional radiology treatment include 1. allergy to iodinated contrast media, 2. severe renal impairment, and 3. anatomic issues such as occlusion of the feeding vessels, 4. limited access (e.g., occluded femoral/iliac arteries), and 5. challenging local vascular anatomy, which may make transcatheter treatment too difficult to perform. However, in general, most VAAs can be treated by interventional radiologists with sufficient experience using modern equipment.
内脏动脉瘤栓塞治疗的基本技术要点:
操作者治疗内脏动脉瘤应具备的能力
CTA在内脏动脉瘤栓塞前是非常重要的。它主要可以了解动脉解剖走行,动脉瘤的位置、大小、解剖特征和病理特征。这些都为选择治疗内脏动脉瘤方案提供依据。如窄颈动脉瘤多考虑弹簧栓子的填塞,而宽颈动脉瘤需要考虑球囊辅助或支架辅助的弹簧栓子填塞,甚至是覆膜支撑架。对于巨大的内脏动脉瘤,由于经济原因或技术上的考虑也多采用覆膜支撑架,除非载瘤动脉走行迂曲或存在支撑架锚区,动脉瘤上有重要分支。此种情况下可考虑多层支撑架的植入。
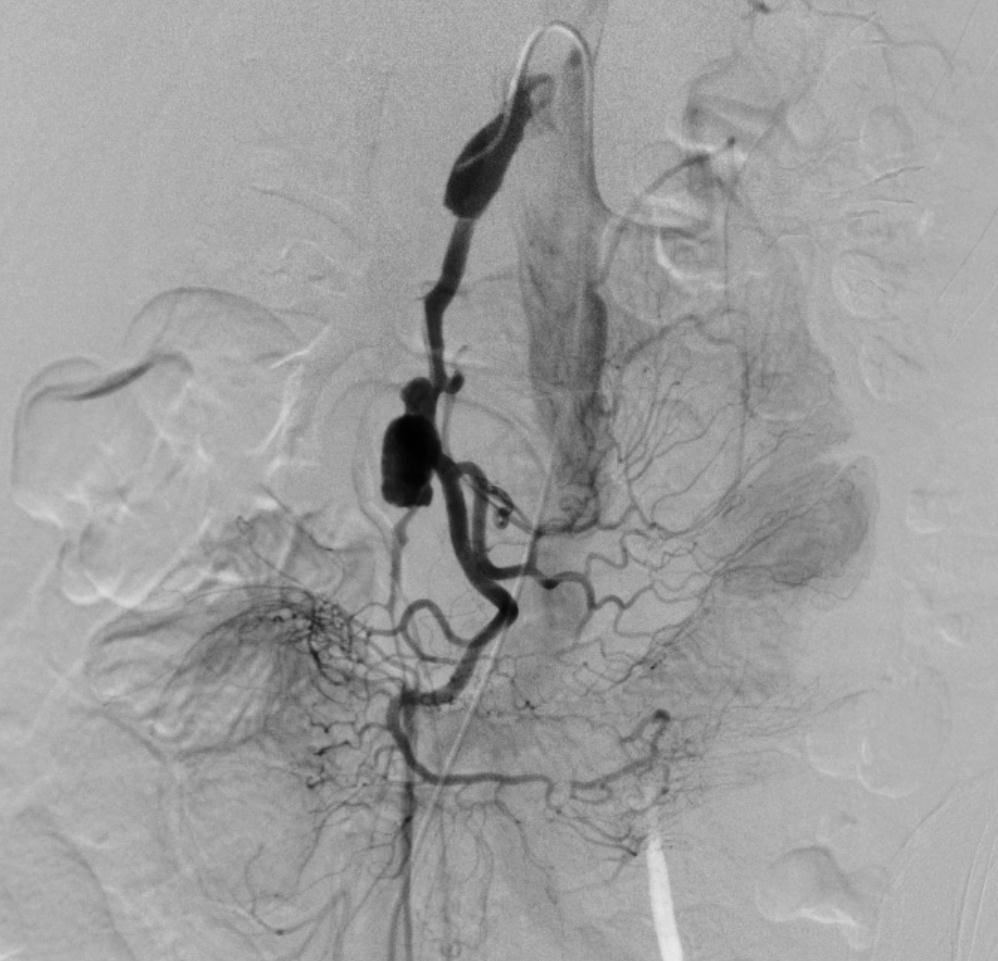
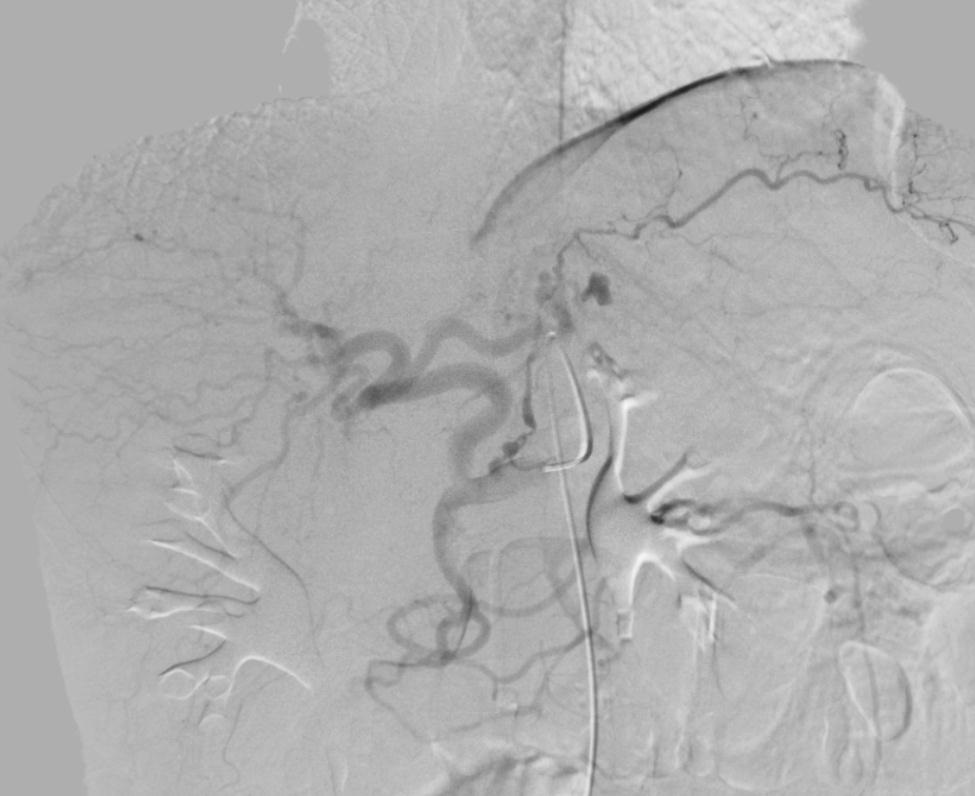
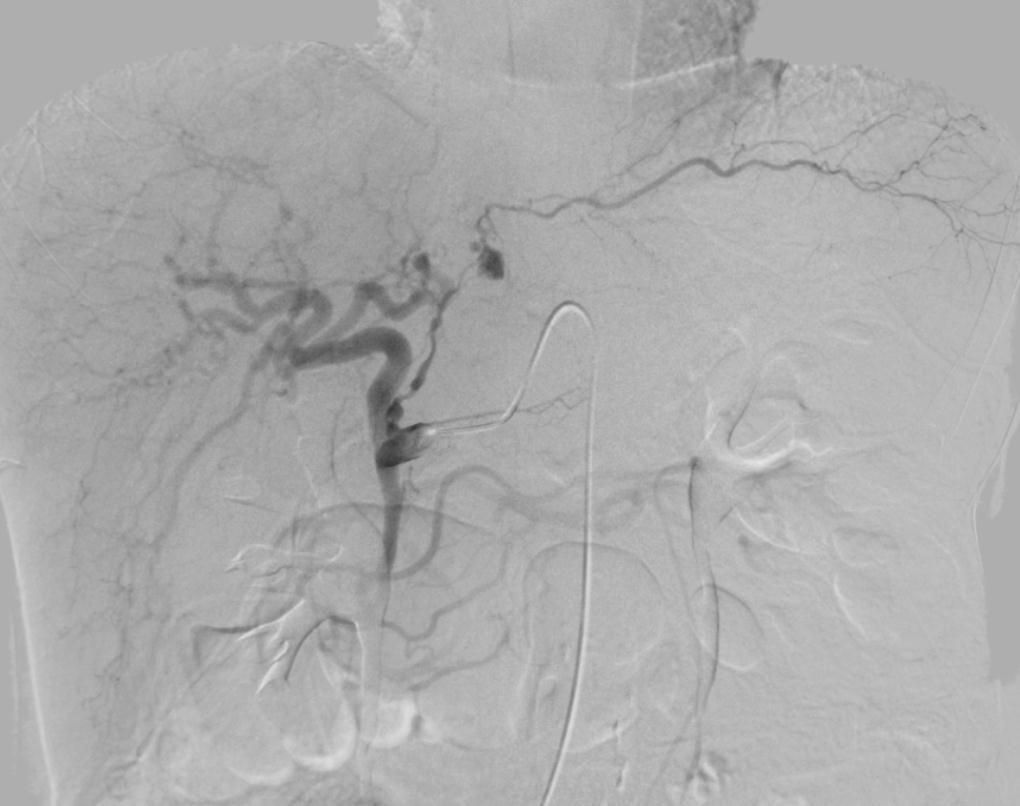
选择合适的6~8F带弯曲的引导导管(guarding catheter)。它的主要作用是稳定工作导管(working catheter)达到靶血管位置(包括动脉瘤开口远端或动脉瘤囊内)。在治疗前首先使用引导导管进行载瘤动脉的初选,如腹腔动脉或肠系膜上动脉。再以共轴导管(coaxial catheter)形式置入工作导管,在导丝的引导下进入更远端的靶血管目标区(例如脾动脉或肠系膜上动脉分支)。通过引导导管的 "Y" 型阀注射造影剂可以在不撤出工作导管的情况下观察内脏动脉瘤治疗前后的情况。引导导管可以通过导丝直接引入覆膜支撑架进入载瘤动脉区域。
选择工作导管的类型主要根据载瘤动脉的走行,例如经股动脉途径选择4~5FCobra进入肠系膜上动脉或脾动脉等。或选择其它适形弯曲导管主要根据操作者的经验。通过工作导管有时可以直接释放弹簧栓子对较大的动脉瘤实施瘤囊填塞。
选择超滑(亲水导丝)、超长、超硬导丝主要目的是利于工作导管达到靶血管区。对于困难的病例包括小动脉瘤,载瘤动脉走行迂曲,常规导管不能达到靶血管目标区域,可考虑使用微导管,形成三轴导管(triaxial catheter)可以稳定地将导管送到目标血管。
动脉瘤的弹簧栓的栓塞主要包括两种技术包括 trapping 技术和 parking 技术。前者又称为三明治技术(sandiwich technology)和backdoor-frontdoor techonology);后者被称为瘤囊填塞技术。
trapping 技术是最常应用的技术。最适合末梢动脉瘤超选择栓塞,宽大或大的动脉瘤。往往需要使用微导管。再通非常罕见,主要缺点是需要阻塞载瘤动脉的血流,潜在导致相关的器官功能暂时或永久下降。包括支撑架辅助或球囊辅助在内的动脉瘤囊栓塞技术(parking technology)仅适合小动脉瘤或窄颈动脉瘤。 为了防止弹簧栓子在释放过程中出现偏离(Coil Deviation) 1. 在高血流和大血管中用球囊控制血流 2. 当球囊不能够进入靶血管,可以进行弹簧栓子锚定(Coil anchor)
3. 动脉瘤隔离栓塞术前,多个弹簧栓子锚定动脉瘤末端,防止弹簧栓子偏离
覆膜支撑架技术往往使动脉瘤上分支或支撑架锚区的分支动脉不得不阻塞。覆膜支撑架的柔顺度较差,对载瘤动脉走行要求较高,主要用于载瘤动脉走行比较平滑的宽颈动脉瘤实施治疗。
多层支撑架的样本量目前还比较少。
液体栓塞剂既可以单独用于动脉瘤囊内的填塞,也可以与支撑架联合应用。除了可以增加治疗的效果(填塞的致密性),也可以省钱。
周围血管动脉瘤栓塞后的抗菌素应用非常重要。因为一旦感染后果非常严重。 血管内治疗完全消除动脉瘤的失败率在4%-43%,外科择期修补手术的死亡率<0.5%。 介入治疗的随访面临影像学的困境,如很多栓塞剂弹簧栓子、Onyx胶在随访影像上制造伪影妨碍随访的判断,掩饰实质脏器的灌注现象和瘤囊的生长。目前没有血管内治疗后影像工具选择的共识,可能的随访影像包括MRA、CTA、超声或这些检查工具的联合应用。随访间隔每1、3、6个月,或者更密切,取决于位置和手术技术成功与否,但推荐每年随访一次。
Nonsurgical treatment of VAA is carried out with the patient under local anesthesia and light sedation. General anesthesia is rarely required. Hospital stay after treatment
is minimal, and most patients are discharged home the next day.
1. Berceli et al. Semin Vasc Surg 2005;18:196
2. Messina et al. Surg Clin North Am 1997;77:425
3. Heestand et al. Am Surg 2003;69:933
4. Stanley et al. Cardiol Clin 2002;20:611
5. Abbas et al. Ann Vasc Surg 2002; 16:422
|