外科治疗作为一种局部治疗,根据肝转移的数目,在结直肠癌肝转移治疗的中位生存期为28~59个月,5年生存率是25~51%(中位=36)[1]。1~3个转移的5年生存期25.9~50%(中位 39%)。≥4个转移,5年生存率0%~53%(中位 17%)。
局部消融治疗改善病人的生存吗?【2】
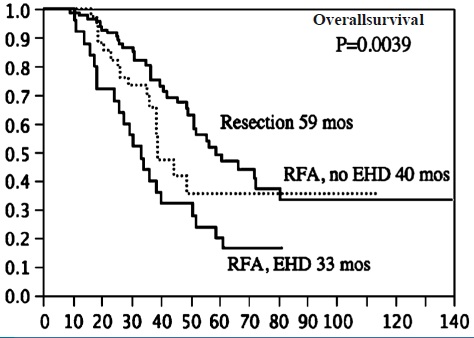
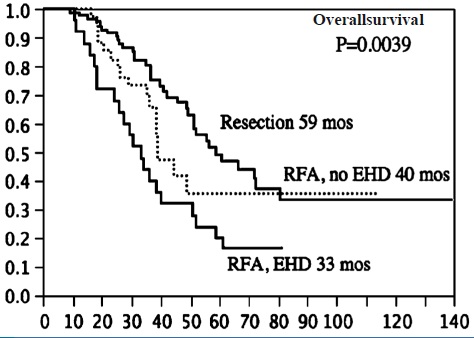
These data provide evidence that when complete resection cannot be achieved, selective use of RFA can provide a modest survival benefit over chemotherapy alone for patients with colorectal metastases confined to the liver.
The higher local recurrence rate, higher intrahepatic failure rate, and associated lower recurrence-free and overall survival rate for patients treated with RFA as a component of therapy compared with resection alone could not be explained by differences in the known patient, primary tumor, liver tumor, or perioperative factors, which predict recurrence and survival for patients treated surgically for colorectal metastases. Although patient selection for RFA may bias the analysis, selection was based on anatomy, not biology, as known risk factors for survival were not different among studied groups, but survival even in the subgroup of patients with solitary tumors treated with RFA was lower than the group treated with resection.
The proliferation of ablation techniques such as RFA for treatment of metastatic liver tumors has unfortunately preceded the analysis of outcome for the treatment modality. Proposal for a randomized trial comparing RFA versus resection for potentially resectable colorectal liver metastases must take into consideration existing data, such as these and may be inappropriate at this time.
Abdalla EK, Ann Surg 2004
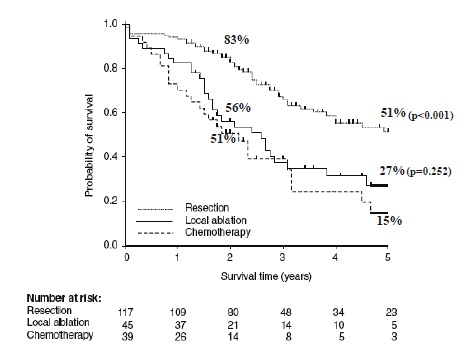
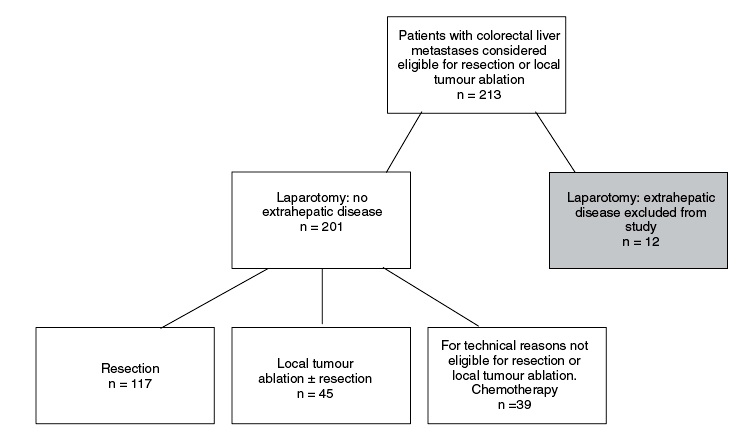
局部消融治疗可以改善病人的生存吗?【3】RuersT, Ann SurgOncol 2007
Although overall survival did not reached statistical significance, the median DFS of 9 months suggests a beneficial effect of local tumour ablation for non-resectable colorectal liver metastases. Moreover, compared with systemic chemotherapy more QALY's were gained after local ablative therapy.
外科/射频消融的预期因素
This study shows that, although patients in both groups had a solitary liver metastasis, other factors including medical comorbidities, technically challenging tumor locations and extra-hepatic disease were different, prompting selection of therapy. With a simultaneous ablation program, higher risk patients have been channeled to RFA, leaving a highly selected group of patients for resection with a very favorable survival. RFA still achieved long-term survival in patients who were otherwise not candidates for resection.
* 统计学的异质性 mata分析中,不可避免地,纳入同一个Meta分析的所有研究都存在差异。将Meta分析中不同研究间的各种变异,称之为异质性。Cochrane 网站的术语网页中将异质性定义[6]为:① 广义上描述参与者、干预措施和一系列研究间测量结果的差异和多样性,或那些研究中内在真实性的变异。② 专指统计学异质性,用来描述一系列研究中效应量的变异程度,也用于表明除仅可预见的偶然机会外研究间存在的差异性。
1. MD Smith and JL McCall. Systematic review of tumour number and outcome after radical treatment of colorectal liver metastases. Br J Surg. 2009 Oct;96(10):1101-13. doi: 10.1002/bjs.6735. |