DIPS(Direct Intrahepatic Portacaval Shunt)是“直接经肝门腔静脉分流术”的英文缩写。它是为了减少传统TIPSS(Transjugular intrahepatic portosystemic stent shunt)操作的缺陷而设计的一种改良介入技术。
传统TIPSS的技术成功率高(可达95%~99%),并发症发生率低(3%~8%),操作相关的死亡率低(0.5%~1%)。对急诊静脉曲张破裂出血的即刻止血成功率可达90%~99%;不同文献对预防复发出血6个月、1年和2年的有效率分别为85%~90%,70%~85%和45%~70%。TIPSS术后1~2年(平均18个月)复发出血率低于经内镜下治疗,而且对门静脉高压症所致的顽固性腹水有一定疗效[1~12]。
但TIPSS的中远期(≥1年)疗效并不理想。术后再出血1年、2年的发生率分别为为20%~26%,和32%~41%。影响长期疗效的主要因素是术后分流道狭窄或闭塞,75%是发生在支撑架在肝静脉出口位置[4,8,15,23,26,42,43]的狭窄,导致整个肝内分流通道慢性失效。若以复发出血或/和影像学检查为依据,术后6个月、12个月内发生率分别为为17%~25%和23~87%不等[11~21]、而病理标本或尸检的发生率为40%~48%。
为了防止TIPSS术后支撑架内再狭窄,有关技术改进一直在进行[8,22]。以介入放射学角度主要采取两种策略:(1)覆盖分流通道(Covering the shunt),即植入覆膜支撑架到分流通道内,减少传统裸支撑架内膜增生引起的支撑架内狭窄;(2)避开或减少分流通道内肝实质部分(Avoiding the liver),避开肝静脉建立直接的门-腔静脉分流。DIPS和经皮腹膜后脾肾静脉分流术(Percutaneous Retroperitoneal Splenorenal Shunt,PRESS)、经皮肝外门腔分流术(Percutaneous Extrahepatic Portocaval Shunt,PEPS)以及经静脉肝外门腔分流术(Transvenous Extrahepatic Portocaval Shunt,TEPS)一样是基于后一种策略考虑。
DIPS技术是传统TIPSS技术的改良,主要是在肝后段下腔静脉(Retrohepatic segmental of inferior vena cava,RHSIVC)紧邻肝静脉出口的地方与门静脉或门静脉分支之间直接建立低阻力的分流通道,将部分门静脉血流分流到下腔静脉,以达到降低门静脉压力。由于避免传统TIPS经肝静脉建立分流通道,从而减少分流通道的狭窄或闭塞的发生率,把持支撑架相对长期的通畅性[36]。下腔静脉是人体直径最大的静脉,其直径远超过肝静脉,理论上下腔静脉作为门腔静脉分流的出口将改善经肝门腔静脉分流术的通畅率[24~28]。目前主要应用于TIPS术中缺乏肝静脉开口(Budd-Chiari Syndrom[26])或肝硬化肝脏缩小导致肝静脉与门静脉主要分支之间角度过小,不宜从肝静脉穿刺门静脉[25,29],以及前次TIPSS阻塞时[30]。除了扩大TIPSS的适应症,最希望达到的目的是希望获得更为稳定和长期的分流通道开通率。
肝硬化病人,肝静脉引流到下腔静脉几乎是直角或由于严重的肝硬化,门静脉的水平提高几乎与肝静脉水平接近。临床上RUPS-100穿刺组件以产品设计的角度难以经肝静脉穿刺进入门静脉[24]。比较传统的TIPSS,DIPS从门静脉分流到腔静脉的角度小,符合门静脉血流动力学分布,静脉流出道阻塞或狭窄的触发因素比TIPSS少[39],所以分流通道潜在开放的时间比TIPSS长。
就解剖而言,肝硬化患者左叶代偿肥大,为穿刺点的选择和超声引导提供方便[38]。
DIPS的主要缺点和包括外科手术一样属于非选择性分流,术后可因门静脉灌注下降导致进行性肝功能衰竭以及肝性脑病;手术要求置入支架定位精确,支撑架两端不宜在门静脉主干和下腔静脉内伸入过长;有潜在增加肝移植的困难程度;发生腹腔内出血的比例高于常规TIPS;与TIPSS比较增加栓塞胃冠状静脉/胃短静脉的技术难度。
DIPS穿刺技术[34,35]
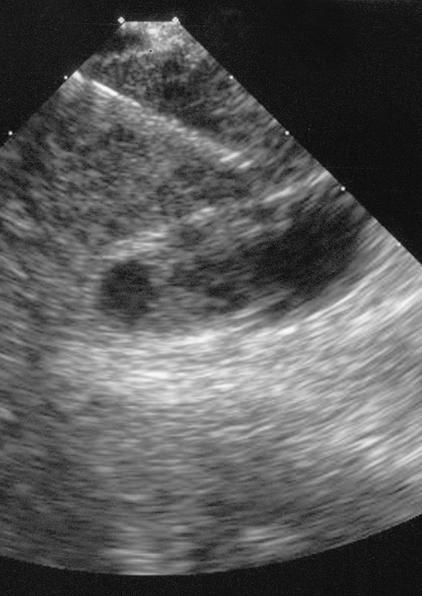
首先将血管内超声探头从右股静脉前进到肝内段下腔静脉。RUPS-100经颈静脉入路引入到下腔静脉(需增加弯度[26]。血管内超声引导下引导穿刺针从下腔静脉进入门静脉最近的分支。超声引导下的DIPS的主要优点是穿刺门静脉时可以直接看到穿刺针的进入轨迹,避免了传统TIPSS盲穿门静脉的缺点,潜在改善了这一位置操作的安全性和有效性。
时利民[40],罗剑军[41]等曾研究肝后段下腔静脉建立肝内分流的影像学研究。周云[37]等人报告采用二维超声引导下穿刺获得成功。
Direct Intrahepatic Portacaval Shunt -DIPS
|
|

|
| 超声引导下门静脉穿刺 |
超声引导下穿刺针进入门静脉时情形 |
穿刺门静脉成功后,5F猪尾巴导管进入门静脉实施门静脉造影。撤出猪尾巴导管置换直径6mm,长6cm球囊扩张导管(Opta 5; Cordis, Miami Lakes, Fla)位于腔静脉与门静脉之间。扩张球囊可以显示近端切迹为下腔静脉壁,远端切迹为门静脉壁。两个切迹之间是的距离是门静脉和下腔静脉之间的肝实质通道的长度,也是支撑架的覆膜部分的最小长度。
测量好切迹间的距离后,充分扩张球囊至两个球囊切迹消失,收缩球囊沿导丝撤出球囊后置换10F鞘管进入门静脉,在透视和血管超声监测下植入覆膜血管支撑架完成直接分流的建立,并造影证实。植入覆膜支撑架是由于以前的研究证实PTFE覆膜支撑架由于裸金属支撑架,可以减少胆汁瘘和肝实质通道内狭窄[31~33]
除了经肝后下腔静脉直接穿刺肝内静脉,也有考虑经皮经肝门静脉穿刺肝后段下腔静脉[38]。
(未完待续)
1. Tripathi D, Therapondos G, Jackson E, Redhead DN, Hayes PC. The role of the transjugular intrahepatic portosystemic stent shunt (TIPSS) in the management of bleeding gastric varices: clinical and haemodynamic correlations. Gut 2002; 51: 270-274
2. Schepke M, Sauerbruch T. Transjugular portosystemic stent shunt in treatment of liver diseases. World J Gastroenterol 2001; 7: 170-174
3. Teng GJ, Bettmann MA, Hoopes PJ, Yang L. Comparison of a new stent and Wallstent for transjugular intrahepatic portosystemic shunt in a porcine model. World J Gastroenterol 2001; 7: 74-79
4. RÖch J, Keller FS. Transjugular intrahepatic portosystemic shunt: present status, comparison with endoscopic therapy and shunt surgery, and future prospectives. World J Surg 2001; 25: 337-346
5. LaBerge JM, Ring EJ, Gordon RL, Ring EJ, Lake JR, Doherty MM, Somber KA, Roberts JP, Asher NL. Creation of transjugular intrahepatic portosystemic shunts with the wallstent endoprosthesis: results in 100 patients. Radiology 1993; 187: 413-420
6. Ugolotti U, Larini P, Marcato C, Saccani A, Puccianti F, Pedretti G. Is the tantalum strecker stent suitable for TIPS creation? short- and mid-term results in 20 consecutive patients. Cardiovasc Intervent Radiol 1997; 20: 38-42
7. Hirota S, Ichikawa S, Matsumoto S, Motohara T, Fukuda T, Yoshikawa T. Interventional radiologic treatment for idiopathic portal hypertension. Cardiovasc Intervent Radiol 1999; 22: 311-314
8. Rossle M, Siegerstetter V, Huber M, Ochs A. The first decade of the transjugular intrahepatic portosystemic shunt (TIPS): state of the art. Liver 1998; 18: 73-89
9. Sanyal AJ, Freedman AM, Luketic VA, Purdum PP, Shiffman ML, Tisnado J, Cole PE. Transjugular intrahepatic portosystemic shunts for patients with active variceal hemorrhage unresponsive to sclerothreapy. Gastroenterology 1996; 111: 138-146
10. Shiffman ML, Jeffers L, Hoofnagle JH, Tralka TS. The role of transjugular intrahepatic portosystemic shunt for treatment of portal hypertension and its complications: a conference sponsored by the National Digestive Diseases Advisory. Board. Hepatology 1995; 22: 1591-1597
11. Feu F, GarcÍ-Pag� JC, Bosch J, Luca A, Teres J, Escorsell A, Rodes J. Relation between portal pressure response to pharmacotherapy and risk of recurrent variceal haemorrhage in patients with cirrhosis. Lancet 1995; 346: 1056-1059
12. Haskal ZJ. Improved patency of transjugular intrahepatic portosystemic shunts in humans: creation and revision with PTFE stent-grafts. Radiology 1999; 213: 759-766
13. Sterling KM, Darcy MD. Stenosis of transjugular intrahepatic portosystemic shunts: presentation and management. AJR 1997; 168: 239-244
14. Lind CD, Malisch TW, Chong WK, Richards WO, Pinson CW, Meranze SG, Mazer M. Incidence of shunt occlusion or stenosis following transjugular intrahepatic portosystemic shunt placement. Gastroenterology 1994; 106: 1277-1283
15. Ong JP, Sands M, Younossi ZM. Transjugular intrahepatic portosystemic shunts (TIPS): A decade later. J Clin Gastroenterol 2000; 30: 14-28
16 RÖsle M, Haag K, Ochs A, Sellinger M, NÖdge G, Perarnau JM, Berger E, Blum V, Gabelmann A, Hauenstein K, Langer M, Gerok W. The transjugular intrahepatic portosystemic stent-shunt procedure for variceal bleeding. N Engl J Med 1994: 330: 165-171
17. Hausegger KA, Sternthal HN, Klein GE, Karaic R, Stauber R, Zenker G. Transjugular intrahepatic portosystemic shunt: angiographic follow-up and secondary interventions. Radiology 1994; 191: 177-181
18. Laberge JM, Somberg KA, Lake JR, Gordon RL, Kerlan RK, Ascher NL, Roberts JP, Simor MM, Doherty CA, Hahn J, Bacchetti P, Ring EJ. Two-year outcome following transjugulr intrahepatic portosystemic shunt for variceal bleeding: results in 90 patients. Gastroenterology 1995; 108: 1143-1151
19. Latimer J, Bawa SM, Rees CJ, Hudson M, Rose JDG. Patency and reintervention rates during routine TIPSS surveillance. Cardiovasc Intervent Radiol 1998; 21: 234-239
20. Jalan R, Forrest EH, Stanley AJ, Redhead DN, Forbes J, Dillon JF, Macgilchrist AJ, Finlayson NDC, Hayes PC. A randomized trial comparing transjugular intrahepatic portosystemic stent-shunt with variceal band ligation in the prevention of rebleeding from esophageal varices. Hepatology 1997; 26: 1115-1122
21. Sauer P, Theilmann L, Stremmel W, Benz C, Richter GM, Stiehl A. Transjugular intrahepatic portosystemic stent shunt versus sclerotherapy plus propranolol for variceal rebleeding. Gastroenterology 1997; 113: 1623-1631
22. Coldwell DM, Ring EJ, Rees CR, et al. Multicenter investigation of the role of transjugular intrahepatic portosystemic shunt in management of portal hypertension. Radiology 1995;196:335–340
23. Murphy TP, Beecham RP, Kim HM, Webb MS, Scola F. Long-term follow-up after TIPS: use of doppler velocity criteria for detecting elevation of the portosystemic gradient. J Vasc Interv Radiol 1998; 9: 275-281
24. Soares GM, Murphy TP. Transcaval TIPS: indications and anatomic considerations. J Vasc Interv Radiol 1999; 10: 1233-1238
25. Huimin L, Gansheng F, Jianyong Y. The anatomic study of imageology related to TIPS. Chin J Radiol 1998; 32: 243-246
26. Petersen B, Uchida BT, Timmermans H, Keller FS, RÖch J. Intravascular us-guided direct intrahepatic portacaval shunt with a PTFE-cov ered stent-graft: feasibility study in swine and initial clinical results. J Vasc Interv Radiol 2001; 12: 475-486
27. Chang RW, Shan-Quan S, Yen WW. An applied anatomical study of the ostia venae hepaticae and the retrohepatic segment of the inferior vena cava. J Anat 1989; 164: 41-47 (abstract)
28. Camargo AM, Teixeira GG, Ortale JR. Anatomy of the ostia venae hepaticae and the retrohepatic segmentt of the inferior vena cava. J Anat 1996; 188: 59-64
29. Gasparini D, Forno MD, Sponza M, Branca B, Tonintto P, Marzio A, Pirisi M. Transjugular intrahepatic portosystemic shunt by direct transcaval approach in patients with acute and hyperacute Budd-chiari syndrome. Eur J Gastroenterol Hepatol 2002; 14: 567-571
30. Seong CK, Kim YJ, Shin TB, Park HY, Kim TH, Kang DS. Transcaval TIPS in patients with failed revision of occluded previous TIPS. Korean J Radiol 2001; 2: 204-209
31. Gandini R, Konda D, Simonetti G. Transjugular intrahepatic portosystemic shunt patency and clinical outcome in patients with Budd-Chiari syndrome: covered versus uncovered stents. Radiology 2006;241:298–305.
32. Charon JP, Alaeddin FH, Pimpalwar SA, et al. Results of a retrospective multicenter trial of the Viatorr expanded polytetrafluoroethylene-covered stent-graft for transjugular intrahepatic portosystemic shunt creation. J Vasc Interv Radiol 2004;15:1219–1230
33. Hernandez-Guerra M, Turnes J, Rubinstein P, et al. PTFE-covered stents improve TIPS patency in Budd-Chiari syndrome. Hepatology 2004;40:1197–1202.
34. Petersen B, Binkert C. Intravascular ultrasound-guided direct intrahepatic portacaval shunt: midterm follow-up. J Vasc Interv Radiol 2004;15:927–938.
35. Petersen B. Intravascular ultrasound-guided direct intrahepatic portacaval shunt: description of technique and technical refinements. J Vasc Interv Radiol 2003;14:21–32.
36. Petersen BD, Clark TW. Direct intrahepatic portocaval shunt. Tech Vasc Interv Radiol. 2008 Dec;11(4):230-4.
37. 周云,陈松旺,宋进华,顾建平 超声在经皮穿刺直接性门腔静脉分流术中的应用. 中国介入影像与治疗学 2011年 第8卷第6期 469页
38. 颜志平.经皮穿刺直接性门腔静脉分流术.中国介入影像与治疗学 2005.2(5):325~328
39. Yu SP, Chu GL, Yang JY, He L, Wang HQ. Direct intrahepatic portocaval shunt through transhepatic puncture via retrohepatic inferior vena cava: applied anatomical study. Surg Radiol Anat. 2009 Jun;31(5):325-9. Epub 2008 Dec 16.
40. 时利民 何少武 刘新 李慎江 丁明权 王永清 张传森 纪荣明 蒋尔鹏 经皮穿刺直接性门腔静脉分流术的影像学研究 实用医药杂志2007年 07月 第24卷 第07期 769页
41. 罗剑钧, 颜志平,周康荣,等. 经肝后段下腔静脉建立肝内门腔分流的CT研究. 临床放射学杂志, 2002, 21(11): 893.(此中国作者还发表一篇 Luo JJ, Yan ZP, Zhou KR, Qian S. Direct intrahepatic portacaval shunt: an experimental study. World J Gastroenterol. 2003 Feb;9(2):324-8.)
42. Saxon RS, Ross PL, Mendel-Hartvig J, Barton RE, Benner K, Flora K, Petersen BD, Lakin PC, Keller FS. Transjugular intrahepatic portosystemic shunt patency and the importance of stenosis location in the development of recurrent symptoms.Radiology. 1998 Jun;207(3):683-93.
43. Haskal ZJ, Pentecost MJ, Soulen MC, Shlansky-Goldberg RD, Baum RA, Cope C. Transjugular intrahepatic portosystemic shunt stenosis and revision: early and midterm results. AJR Am J Roentgenol. 1994 Aug;163(2):439-44. |

