股动脉支撑架植入早期已发表的数据提示,在股腘动脉段置入支架与首选PTA相比没有优势。
早期血管支架 vs PTA 没有显著性差异
在比较股腘动脉闭塞的首选支架置入治疗与球囊扩张治疗的荷兰随机试验中,Vroegindeweij 等人【D Vroegindeweij 1997】将患者随机分入首选支架置入(n=24)组与PTA(n=27)组。1年累积临床和血液动力学成功率对支架置入为74%,对PTA为85%(P=.25)。用彩色血流多普勒超声评估的1年初次通畅率对支架组患者为62%,PTA治疗组为74%(P=.22)。第一年,闭塞发生于5例支架治疗患者(21%),而PTA组为2例。他们作出结论,与PTA比较,支架置入并未改善临床与血液动力学结果,而且同时,支架治疗组患者的闭塞率更高。
在Henry等人【Henre M 1995】使用股腘动脉Palmaz支架治疗的126名患者系列中,报告的4年通畅率为65%,但平均病变长度为3.8cm,且对使用2个或更多支架的长节段病变及使用直径5或6mm的支架与7mm的支架之间通畅率是有显著差异的。换句话说,这些更好的结果是在单独使用PTA也期待会有极好结果的患者中获得的,没有明确的证据支架改善通畅率。
早期血管支架的价值可在于对PTA失败后果的改善
如同髂动脉段病变,支架的价值可在于对PTA失败后果的改善。
在美国Wallstent支架试验中,90名患者治疗了105处股腘动脉病变,主要是由于PTA疗效不满意。大多数患者为跛行者。平均治疗前ABI为.68。闭塞的平均长度为9.4cm,狭窄为3.7cm。对因PTA失败而治疗的患者,平均ABI升至.96。即而,初次通畅率1年为61%,2年为49%。二次通畅率1年为84%,2年为72%。股腘动脉支架置入的并发症率为髂动脉支架置入的几乎四倍,且与Coumadin(华法令)的使用特别相关。
Cleveland 门诊部的Gray和Olin用支架治疗了55名有长段股浅动脉病变和更严重的临床缺血的首次血管成形术失败的患者;75%使用了Wallstent支架,21%使用了Palmaz支架,4%两者均使用了。平均病变长段为16.5cm,休息时踝-臂指数为0.48+/-0.19。50%的患者有严重缺血。踝-臂指数改善为0.71+/-0.23(P=.001);13.8月时获取的临床受益率为56%。12个月时的初次和二次通率分别为22%和46%。相同的情况出现。在解剖和临床环境不太理想的情况下,支架置入的持久成功率要低得多【Gray BH 1997】。
如北美Wallstent支架系列研究所示,在适宜行PTA(如跛行者)而PTA失败的患者中,通过支架置入术获得了满意的中期二次通畅率,但是在那个系列研究中,为获得与初次通畅率相比增加23%的两年二次开放率,再次介入治疗对许多患者是必需的。对有更严重病变例如Cleveland门诊部系列的患者,疗效明显较差。外科血管置换术适宜于长节段股腘动脉病变,而支架置入用于肢体严重缺血无法行外科手术而血管成形术首次失败的患者。
至今,支架置入的长期疗效没有像PTA那样的仔细记录。因而,没有各种系列结果的表格提供给支架置入术。Bosch和Hunink提供了一个髂动脉支架系列的表格。关于股腘动脉支架置入术的数个系列研究结果的总结由Gray BH和Olin JW发表。
早期 股浅动脉裸支撑架植入结果
|
证据
|
作者[文献]
|
例数/病变数
|
支架类型
|
病变长度(平均)
|
SFA病变类型
|
术后随访
|
|
6月
|
12月
|
24月
|
|
I |
Saxon[1]
|
28
|
PTA组 N=13
|
|
|
|
|
23%
|
|
PTA+覆膜支撑架 N=15
|
|
|
|
|
87%
|
|
Schillinger[2]
|
104
|
PTA N=36
|
9.2±6.4cm
|
|
50%
|
37%
|
|
|
Nitinol N=68
|
10.1±7.5cm
|
|
75%
|
63%
|
|
|
股动脉支架实验[3]
FAST Trial
|
244
|
PTA N=108
|
4.45cm
|
|
|
|
62.2%
|
|
Luminexx N=136
|
4.52cm
|
|
|
|
67%
|
|
药物洗脱支撑架实验[4,5]
|
57
|
药物洗脱支架(雷帕霉素) N=29
|
8.65cm
|
|
|
|
|
|
裸支架 N=28
|
7.63cm
|
|
|
|
|
|
Scheinert[6]
|
|
|
|
|
|
|
|
|
SIROCCO
|
|
|
|
|
|
|
|
|
IIa
IIb
|
Lammer[7]
|
74/80
|
Gore覆膜支撑架
|
13.1cm
|
TASC A 9
TASC B 49
TASC C 22
|
89.7%
|
78.7%
|
|
|
Cheng[8]
|
55/60
|
Nitinol
|
13.8cm
|
中上段病变13%,远段病变87%;其中闭塞性病变52%
|
73.1%
|
62.6%
|
53.8%
|
|
Lugmayr[9]
|
44/54
闭塞:22
狭窄:32
|
Symphony
|
闭塞:4cm
狭窄:3.2cm
|
|
|
87%
|
85%
|
|
Jahnke[10]
|
28/40
|
IntraCoil Nitinol
|
3.6cm
|
SFA 36
腘动脉 4
A/B型
|
|
97.1%
|
86.2%
|
|
Jahnke[11]
|
41/52
|
Hemobahn (Gore)
|
10.9cm
|
闭塞: 43
|
84.5%
|
78.4%
|
74.1%
|
|
Cheng[12]
|
76
|
Nitinol
|
16cm
|
|
|
56%
|
35%
|
|
Daenens[13]
|
38/40
|
Hemobahn (Gore)
|
15cm
|
闭塞:25
|
|
66%
|
|
|
Bray[14]
|
54/59
|
Hemobahn (Gore)
|
17.8cm
|
闭塞:31
|
71.3%
|
60.8%
|
|
|
Wiesinger[15]
|
98/107
髂动脉:60
股浅动脉:47
|
SMART
|
髂动脉:4.5cm
股浅动脉:5cm
|
|
89.8%
|
89.8%
|
|
|
Fischer[16]
|
57/60
|
Hemobahn/Viabahn
|
10.7cm
|
闭塞:87%
|
|
80%
|
36、60个月71%、62%
|
|
Lenti[17]
|
150/166
|
aSpire
|
|
闭塞性病变115处,TASC B型101处,TASC C型47处,TASC D型18处
|
|
64%
|
59%
36月:59%
|
|
IIc
|
Vogel[18]
|
41
|
SMART
|
6.69cm
|
TASC B型37例,TASC C型4例
|
95%
|
84%
|
84%
|
|
Mewissen[19]
|
122/137
|
SMART
|
12.2cm
|
TASC A12
TASC B/C 125
闭塞 20
|
92%
|
76%
|
60%
|
|
Rosenthal[20]
|
47
|
aSpire
|
26.2cm
|
|
18月:68.6%
|
|
Sabeti[21]
|
175/175
|
Nitinol N=52
|
5cm
|
|
85%
|
75%
|
65%
|
|
不锈钢支架 N=125
|
9cm
|
|
78%
|
54%
|
34%
|
|
Schlager[22]
|
286
|
Wallsten N=116
|
10.7cm
|
|
|
54%
|
34%(36月,28%)
|
|
|
|
Nitinol N=170
|
13.9cm(smart)
12.5cm(Dynalinc)
|
|
|
80%
|
64%(36月,47%)
|
|
Rosenthal[23]
|
210
|
机械性内膜切除+aSpire
|
28.2cm
|
|
33月:60.6%
|
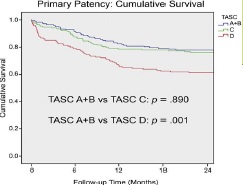
Han 等人比较[26] 股腘动脉TACS 分级血管内治疗初始、辅助初始和二次治疗开放率(secondary patency rate)的结果。TASC A+B 和TASC D型病变的二次治疗开放率没有显著的差异(以下图表)。
2年次级开放率
|
|
TASC A+B |
TASC C |
TASC D |
|
二次治疗开放率 |
86.7% |
85.0% |
78.2% |
早期股浅动脉药物洗脱支撑架的结果
股浅动脉:SIROCCO 研究【Duda SH 2006 Duda SH 2005】
1. 双盲,随机,前瞻,多中心
2. 股浅动脉 Sirolimus 药物洗脱支撑架 vs. 裸SMART 支撑架
3. 结论:>70%狭窄(大于50%,已阻塞病变)
数据表明,在大多数患者中,使用西罗莫司洗脱支架和裸露的SMART支架都是有效的、安全的,并且在长达24个月的时间内不会出现再狭窄。由于裸露支架组的再狭窄率出乎意料地低,因此无法在西罗莫司洗脱支架和裸露的SMART支架之间找到显著差异。
尽管Sirolimus 药物洗脱支架组有效性有所提高的趋势,但在任何变量中都没有统计学显著差异(Sirolimus eluting vs Bare Nitinol stent))。
|
分期
|
I 期
|
II 期
|
|
病例数
|
36
|
57
|
|
长度
|
< 20cm
|
< 14.5 cm
|
|
平均长度
|
8.5 cm
|
8.2 cm
|
|
药物释放速度
|
慢 或 快
|
慢
|
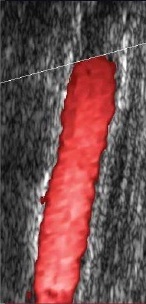
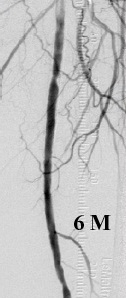
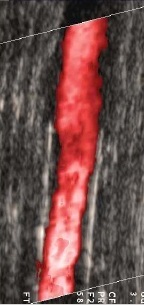
SIROCCO 6月后随访汇集结果影像学表现
|
SIROLIMUS 组 |
SIROLIMUS |
对照组 |
对照组 |
 |
|
|
|
1. Saxon RR, Coffman JM, Gooding JM, et al. Long-term results of ePTFE stent-graft versus angioplasty in the femoropopliteal artery: single center experience from a prospective, randomized trial[J]. J Vasc Interv Radiol,2003,14(3):303-311.
2. Schillinger M, Sabeti S, Loewe C, et al. Balloon angioplasty versus implantation of nitinol stents in the superficial femoral artery[J]. N Engl J Med, 2006,354(18):1879-1888.
3. Krankenberg H, Schlüter M, Steinkamp HJ, et al. Nitinol stent implantation versus percutaneous transluminal angioplasty in superficial femoral artery lesions up to 10 cm in length: the femoral artery stenting trial (FAST) [J]. Circulation, 2007, 116(3):285-292.
4. Duda SH, Bosiers M, Lammer J, et al. Drug-eluting and bare nitinol stents for the treatment of atherosclerotic lesions in the superficial femoral artery: long-term results from the SIROCCO trial[J]. J Endovasc Ther, 2006,13(6):701-710.
5. Duda SH, Bosiers M, Lammer J, et al. Sirolimus-eluting versus bare nitinol stent for obstructive superficial femoral artery disease: the SIROCCO II trial[J]. J Vasc Interv Radiol, 2005, 16(3):331-338.
6. Scheinert D, Scheinert S, Sax J, et al. Prevalence and clinical impact of stent fractures after femoropopliteal stenting[J]. J Am Coll Cardiol,2005,45(2):312-315.
7. Lammer J, Dake MD, Bleyn J, et al. Peripheral arterial obstruction: prospective study of treatment with a transluminally placed self-expanding stent-graft. International Trial Study Group[J]. Radiology, 2000, 217(1):95-104.
8. Cheng SW, Ting AC, Wong J. Endovascular stenting of superficial femoral artery stenosis and occlusions: results and risk factor analysis[J]. Cardiovasc Surg,2001, 9(2):133-140.
9. Lugmayr HF, Holzer H, Kastner M, et al. Treatment of complex arteriosclerotic lesions with nitinol stents in the superficial femoral and popliteal arteries: a midterm follow-up[J]. Radiology, 2002,222(1):37-43.
10. Jahnke T, Voshage G, Müller-Hülsbeck S, et al. Endovascular placement of self-expanding nitinol coil stents for the treatment of femoropopliteal obstructive disease[J]. J Vasc Interv Radiol, 2002,13(3):257-66.
11. Jahnke T, Andresen R, Müller-Hülsbeck S, et al. Hemobahn stent-grafts for treatment of femoropopliteal arterial obstructions: midterm results of a prospective trial[J]. J Vasc Interv Radiol, 2003,14(1):41-51.
12. Cheng SW, Ting AC, Ho P. Angioplasty and primary stenting of high-grade, long-segment superficial femoral artery disease: is it worthwhile? [J]. Ann Vasc Surg, 2003,17(4):430-437.
13. Daenens K, Maleux G, Fourneau I, et al. Hemobahn stent-grafts in the treatment of femoropopliteal occlusive disease[J]. J Cardiovasc Surg (Torino), 2005,46(1):25-29.
14. Bray PJ, Robson WJ, Bray AE. Percutaneous treatment of long superficial femoral artery occlusive disease: efficacy of the Hemobahn stent-graft[J]. J Endovasc Ther, 2003; 10(3):619-628.
15. Wiesinger B, Beregi JP, Oliva VL, et al. PTFE-covered self-expanding nitinol stents for the treatment of severe iliac and femoral artery stenoses and occlusions: final results from a prospective study[J]. J Endovasc Ther,2005,12(2):240-246.
16. Fischer M, Schwabe C, Schulte KL. Value of the hemobahn/viabahn endoprosthesis in the treatment of long chronic lesions of the superficial femoral artery: 6 years of experience[J]. J Endovasc Ther,2006,13(3):281-290.
17. Lenti M, Cieri E, De Rango P, et al. Endovascular treatment of long lesions of the superficial femoral artery: results from a multicenter registry of a spiral, covered polytetrafluoroethylene stent[J]. J Vasc Surg, 2007,45(1):32-39.
18. Vogel TR, Shindelman LE, Nackman GB, et al. Efficacious use of nitinol stents in the femoral and popliteal arteries[J]. J Vasc Surg,2003, 38(6):1178-1184.
19. Mewissen MW. Self-expanding nitinol stents in the femoropopliteal segment: technique and mid-term results[J]. Tech Vasc Interv Radiol,2004, 7(1):2-5.
20. Rosenthal D, Martin JD, Schubart PJ, et al. Remote superficial femoral artery endarterectomy and distal aSpire stenting: multicenter medium-term results[J]. J Vasc Surg, 2004, 40(1):67-72.
21. Sabeti S, Schillinger M, Amighi J, et al. Primary patency of femoropopliteal arteries treated with nitinol versus stainless steel self-expanding stents: propensity score- adjusted analysis[J]. Radiology, 2004, 232(2):516-521.
22. Schlager O, Dick P, Sabeti S, et al. Long-segment SFA stenting--the dark sides: in-stent restenosis, clinical deterioration, and stent fractures[J]. J Endovasc Ther,2005,12(6):676-684.
23. Rosenthal D, Martin JD, Smeets L, et al. Remote superficial femoral artery endarterectomy and distal aSpire stenting: results of a multinational study at three-year follow-up[J]. J Cardiovasc Surg (Torino). 2006; 47(4):385-91.
24. Vroegindeweij D, Vos LD, Tielbeek AV, Buth J, vd Bosch HC. Balloon angioplasty combined with primary stenting versus balloon angioplasty alone in femoropopliteal obstructions: A comparative randomized study. Cardiovasc Intervent Radiol. 1997 Nov-Dec;20(6):420-5. (medline)
25. Henry M, Amor M, Ethevenot G, Henry I, Amicabile C, Beron R, Mentre B, Allaoui M, Touchot N. Palmaz stent placement in iliac and femoropopliteal arteries: primary and secondary patency in 310 patients with 2-4-year follow-up. Radiology. 1995 Oct;197(1):167-74.
26. Han DK, Shah TR, Ellozy SH, Vouyouka AG, Marin ML, Faries PL. The success of endovascular therapy for all TransAtlantic Society Consensus graded femoropopliteal lesions. Ann Vasc Surg. 2011 Jan;25(1):15-24
|