PPH的传统定义是在阴道分娩后24小时内失血大于500ml。随后,更多的临床定义被提出,包括美国妇科和产科学会的定义,PPH为血细胞比容在产前和产后相比有10%下降或需要输红细胞,或者剖宫产后出血超过1000mL。使用不同的定义产后出血的发病率不一样,PPH在阴道分娩中发生率为3.9%,在剖腹产中为6.4%。一种PPH的分类方法是根据分娩的临时关系。早期PPH发生在产后第一个24小时,而晚期PPH发生在超过24小时时间但小于产后6周。
|

|
|
即便是剖宫产后,也会产后大出血 |
产后大出血(Postparturn haemorrhage,PPH)是产科急症,即可来自自然分娩,也可以发生在剖宫产后。尽管产科重症监护和现代技术使和子宫收缩无力以及生殖道撕裂导致的产后大出血显著的下降,但产科大出血是仍然是产后发生的一种严重的并发症。在世界范围内,PPH 是孕妇死亡(Maternal Mortality M&M)的第三位主要原因【1】,出血可导致低血压休克、肾功能衰竭、呼吸窘迫综合征、凝血功能障碍、希罕综合征等。在美国,产后出血(PPH)也是产妇三大主要死亡原因之一(还有肺栓塞和妊高症),占产妇死亡率的13%【2】。但在发达国家和发展中国家这一数据是不一样的,前者为1/100000,后者为1/1000【4】。
保守治疗一直是第一线的防治方法,例如裂伤修复、子宫填塞、纠正凝血功能以及使用宫缩剂。但是一旦这些方法失败,过去很少有方法应付。很多病人常规进行双侧髂内动脉和/或子宫动脉结扎。如果难治性出血继续,需要进行子宫切除术,此后会丧失生育能力。产后大出血也是围产期子宫切除的主要原因之一。 目前理想的治疗方法仍然在争论中。
ACOG(2006)认为,栓塞,稳定病人的持续出血和子宫切除术后的持续出血病人。而实际上对于危及生命的产后大出血栓塞是十分有效的。
|
|
|
“A patient with stable vital signs and persistent bleeding, especially if the rate of loss is not excessive, may be a candidate for arterial embolization. Radiographic identification of bleeding vessels allows embolization with Gelfoam, coils, or glue. Balloon occlusion is also a technique used in such circumstances. Embolization can be used for bleeding that continues after hysterectomy or can be used as an alternative to hysterectomy to preserve fertility.” |
Brown等在1979年首先报道了子宫动脉栓塞术在难治性产后出血的应用;并且马上在1980年Pais等进行了重复。有趣的是,现在的栓塞技术与当时的首次报道并没有大的改变。股动脉的直接穿刺后插入眼镜蛇形导管或者反曲线导管(例如Roberts子宫动脉导管)至髂内动脉的前支,行选择性动脉造影。当找到出血血管后,进行选择性置管,注入有明胶海绵块的混悬浆直至血管内的前进血流中止。选择明胶海绵是因为它只会引起暂时性的血管闭塞,2-4周后血流可以自行再通。
IR and Pelvic Embolization
• Diagnostic angiography well established in the 1960‟s
• Embolotherapy developed from the early 1970‟s
• Pelvic embolization for arterial bleeding in pelvic fractures first described by MGH group in 1972*
• Complex pelvic embolization is now routine due to development of Uterine Fibroid Embolization
–*Arteriography in the management of hemorrhage from pelvic fractures. Margolies MN, Ring EJ, Waltman AC et al. NEJM 1972; 287: 317-321
Embolization in the Treatment of PPH
• First described in the late 1970‟s
• Multiple subsequent articles
• Techniques have become very much more refined over past 22 years
“Uncontrollable postpartum bleeding: a new ap porach to hemostasis through angiographic arterial embolization” Brown et al.Obstet. Gynecol. 1979,54,361-635
– Transcatheter arterial embolization for control of persistent massive puerperal hemorrhage after bilateral surgical hypogastric artery ligation. Heaston D, Mireau D, Brown B et al. AJR 1979; 133: 152-154
– A new approach to hemostasis through angiographic arterial embolization. Brown B, Heaston D, Poulson A et al. Obstetrics and Gynecology 1979; 54: 361-365
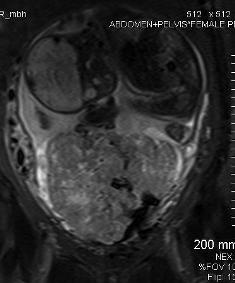
产后大出血危险患者:胎盘前置
|
|
|
强力手法剥离胎盘,导致产后大出血。实施子宫切除术 |
北京协和医院产科自1989.6~1999.6十年间生产总数11401,发生产后大出血的病例为276例,占2.42%【3】,其中15例需要手术干预,占出血病例的5.4%。
1979年首次报告经导管子宫动脉栓塞治疗产后大出血以来【5,6】,产后大出血治疗方法已经有了改变,它以较高的技术成功率和有效性迅速成为治疗原发性和继发性产后大出血的主要选择[7~10]。对于PPH的病人,使用血管造影进行评价和栓塞的方法已经建立,并且被证明是安全有效的。除了其成功率高以外,血管栓塞的最大优点是病人能够保留生育力。 尽管如此,临床上有关产后大出血子宫动脉栓塞仍没有得到充分的应用。很多产科医生对于这一操作的认识仍然是有限的【11】。 2002年一项在英国的调查显示,86%的产科医院严重的产后大出血从来没有应用过子宫动脉栓塞;在其前5年,12%的医院每4例严重PPH进行一例的子宫动脉栓塞【11】。没有充分得到应用的原因包括缺少先进的血管造影设备,经验成熟的24小时值班的团队,和在病人生命体征不稳定的情况下转移病人到血管造影室或有血管造影室医院不可预测的危险【12】。
由于剖腹产病例的不断增加,子宫动脉栓塞对于剖腹产后的PPH有效性的资料也在不断的累积中。
本站将讨论产后出血(PPH)的特殊原因,各种已有方法和新型治疗方法,并评估经导管栓塞治疗这些疾病的效果。
1. Gilbert L, Porter W, Brown VA. Postparturn haemorrhage: a continuing problem.BrJ Obstet Gynecol 1987; 94:67-71.
2. Obstetrical hemorrhage.In: Cunningham FG, Macdonald PC, eds.William's obstet rics.Stamford Connecticut: Appleton & Lange; 1999:745- 769.
3.Liu Juntao et al:Optimal management of postpartum hemorrhage Chinese Medical Journal, 2001, Vol. 114 No. 12 : 1280-1282
4.Allan J Jacobs, MD Causes and treatment of postpartum hemorrhage http://patients.uptodate.com/topic.asp?file=postpart/4483#22
5. B.J. Brown, D.K. Heaston, A.M. Poulson, H.A. Gabert, D.E. Mineau and F.J. Miller Jr, Uncontrollable postpartum bleeding: a new approach to hemostasis through angiographic arterial embolization, Obstet Gynecol 54 (1979), pp. 361–365.
6. D.K. Heaston, D.E. Mineau, B.J. Brown and F.J. Miller Jr, Transcatheter arterial embolization for control of persistent massive puerperal hemorrhage after bilateral surgical hypogastric artery ligation, AJR Am J Roentgenol 133 (1979), pp. 152–154.
7. J.M. Kirby, J.R. Kachura and D.K. Rajan et al., Arterial embolization for primary postpartum hemorrhage, J Vasc Interv Radiol 20 (2009), pp. 1036–1045.
8. C. Touboul, W. Badiou and J. Saada et al., Efficacy of selective arterial embolisation for the treatment of life-threatening post-partum haemorrhage in a large population, PLoS One 3 (2008), p. e3819.
9. J.P. Pelage, O. Le Dref and J. Mateo et al., Life-threatening primary postpartum hemorrhage: treatment with emergency selective arterial embolization, Radiology 208 (1998), pp. 359–362.
10. J.P. Pelage, P. Soyer and D. Repiquet et al., Secondary postpartum hemorrhage: treatment with selective arterial embolization, Radiology 212 (1999), pp. 385–389.
11. H.A. Mousa and Z. Alfirevic, Major postpartum hemorrhage: survey of maternity units in the United Kingdom, Acta Obstet Gynecol Scand 81 (2002), pp. 727–730.
12. N. Ledee, Y. Ville, D. Musset, F. Mercier, R. Frydman and H. Fernandez, Management in intractable obstetric haemorrhage: an audit study on 61 cases, Eur J Obstet Gynecol Reprod Biol 94 (2001), pp. 189–196.
|