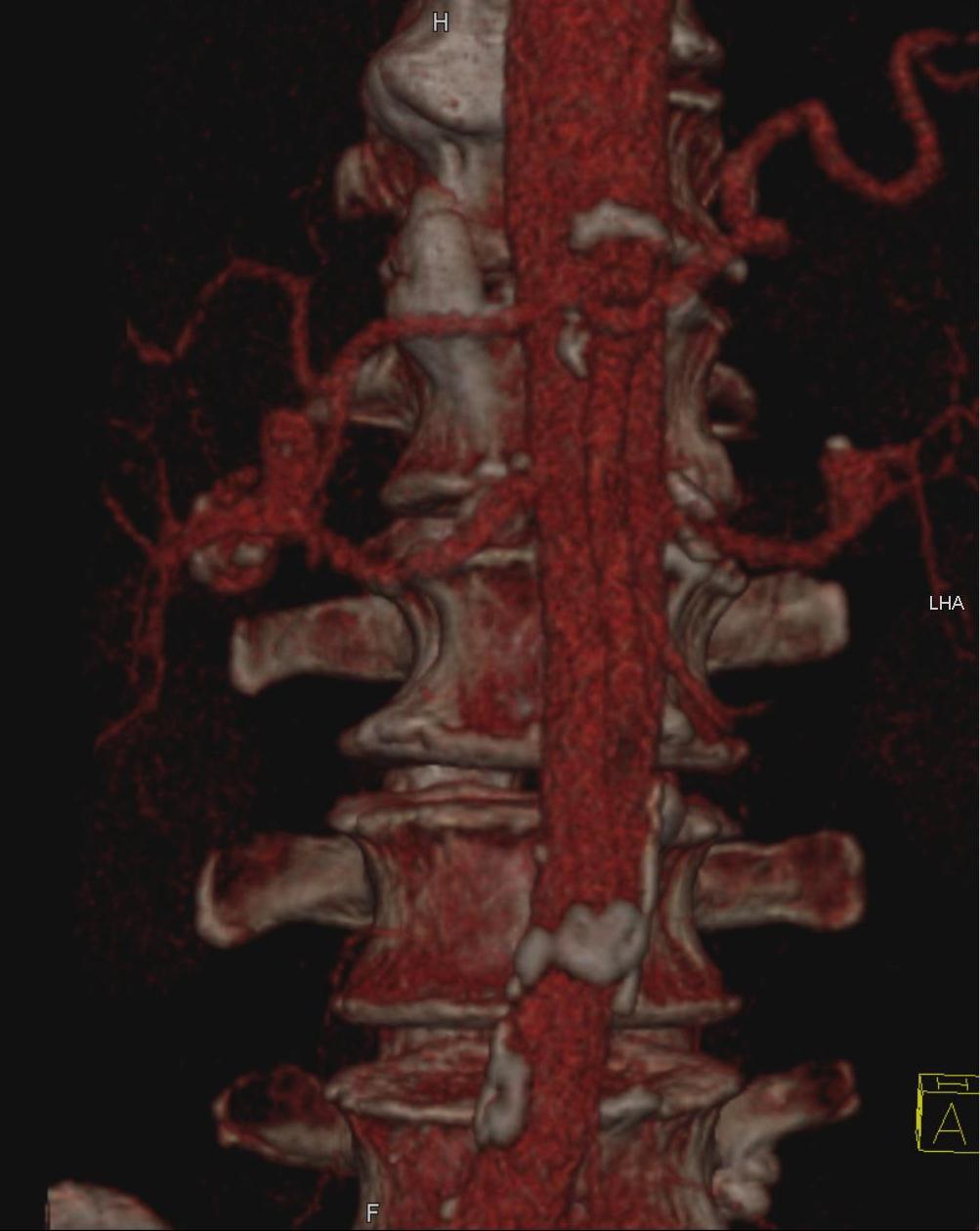
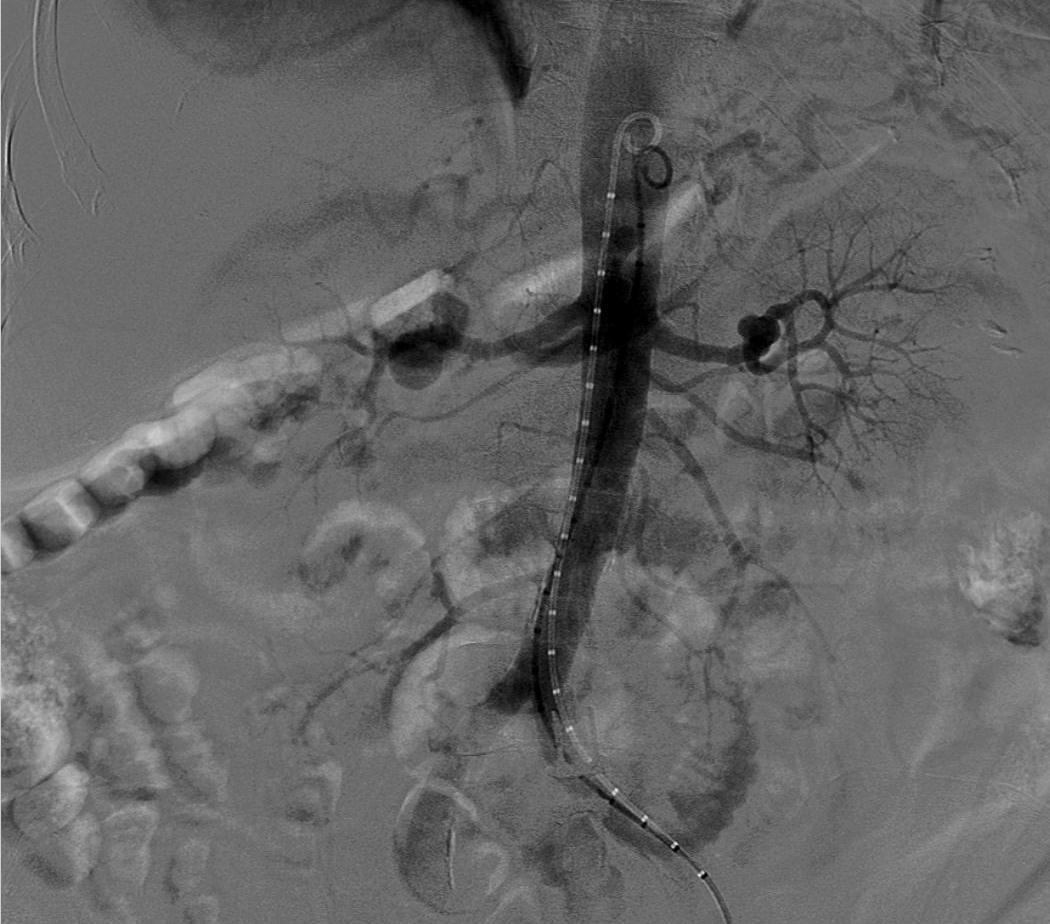
肾动脉瘤治疗的选择包括观察,外科手术,血管内支撑架,血管内栓塞,内科治疗或这些方法的联合治疗。治疗的选择取决于个体化的因素,包括动脉瘤的位置,形态学改变,破裂等因素。
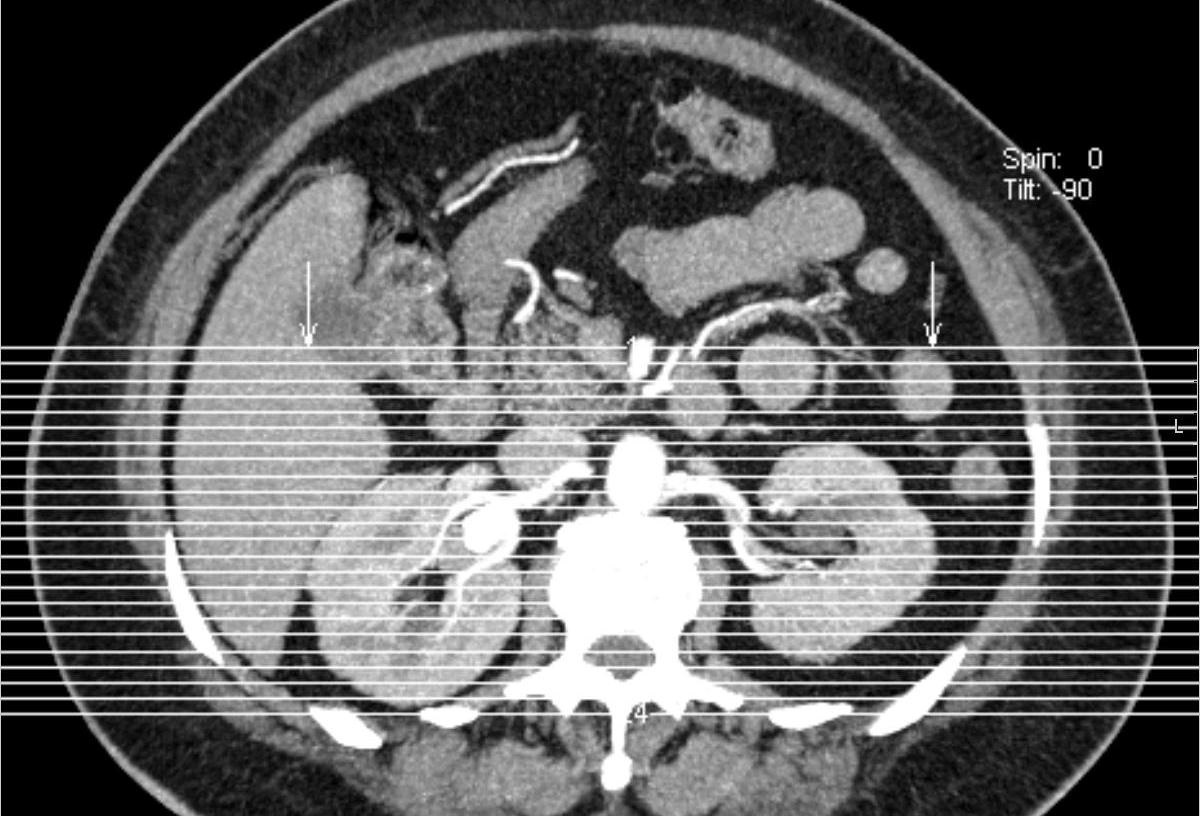
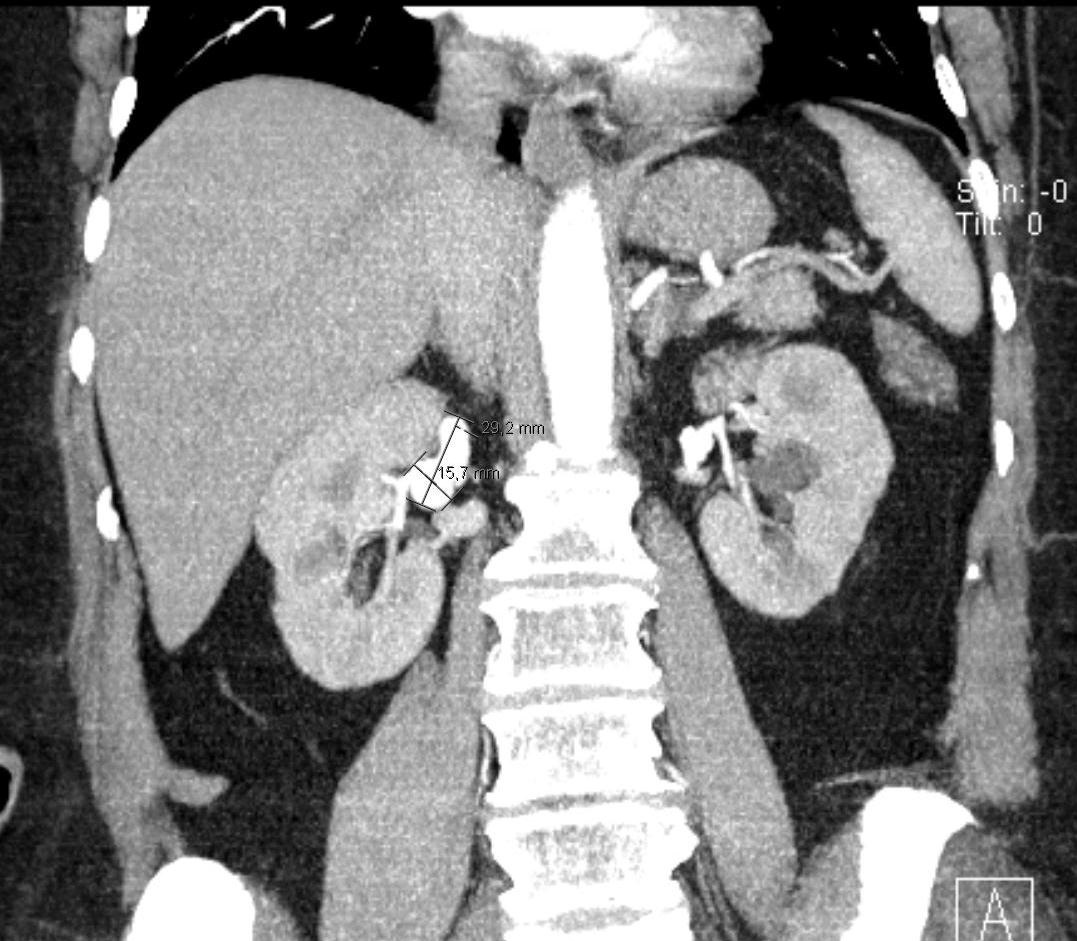
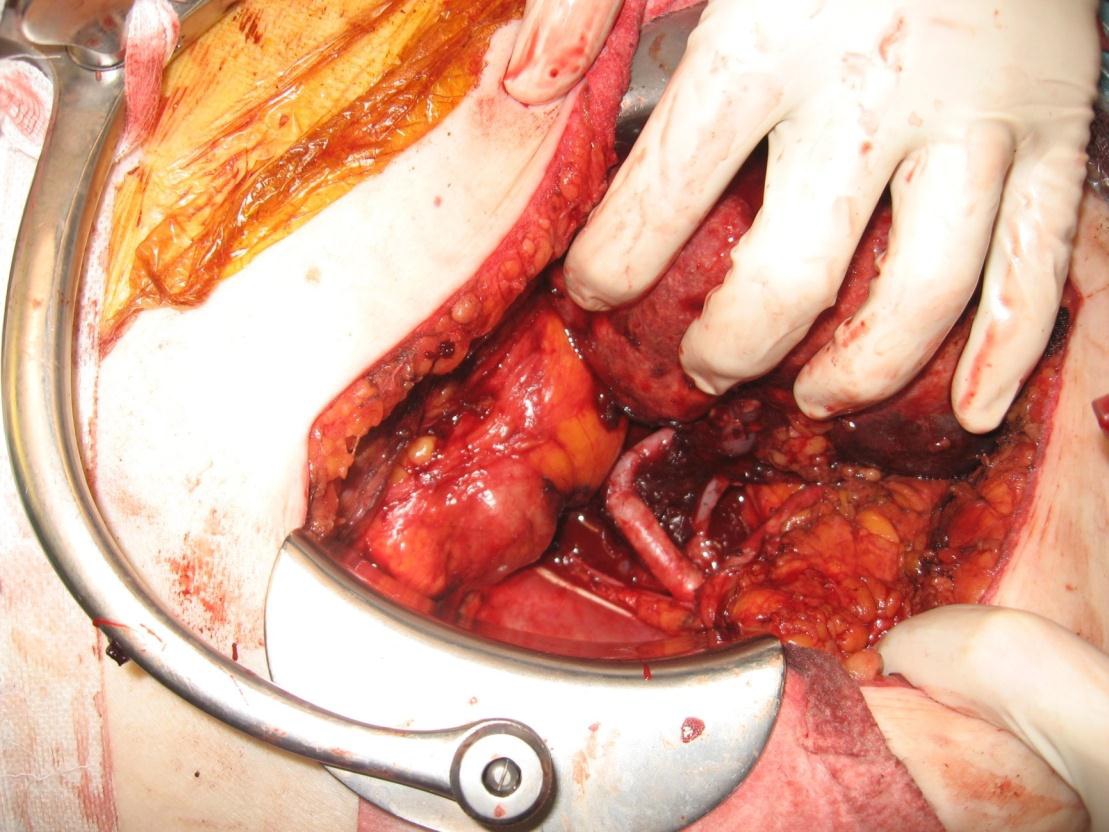
观察是指对无症状的<2厘米直径的肾或肾实质内动脉瘤而言[1~4]。每年对已发现的动脉瘤进行影像学随访,随访的内容包括任何的体积变化,数量的变化和动脉瘤形态的变化。 外科手术包括破裂肾动脉瘤的急诊手术,以及择期肾动脉瘤的手术修补。前者主要是针对已破裂肾动脉瘤控制出血和挽救生命。此情况由于暴露膈下较大血肿使暴露肾动脉较为困难,需要在肾上水平甚至腹腔动脉以上水平的腹主动脉进行暂时性阻断。一旦肾动脉充分暴露,出血得到控制可以松开对腹主动脉的阻断。多数情况下破裂的肾动脉瘤手术由于生命体征不满意不能保留肾脏,肾切除或部分肾切除往往是必须的。只是在生命体征稳定下才可能从容实施肾动脉的重建手术[29]。对于妊娠子宫( gravid uterus )的处理原则是一样的,应尽量避免刨宫产( Cesarean delivery )以免增加手术时间和新的出血。刨宫产只在胎儿窘迫的风险大于胎儿产,已经危及产妇的生命[30,31]。
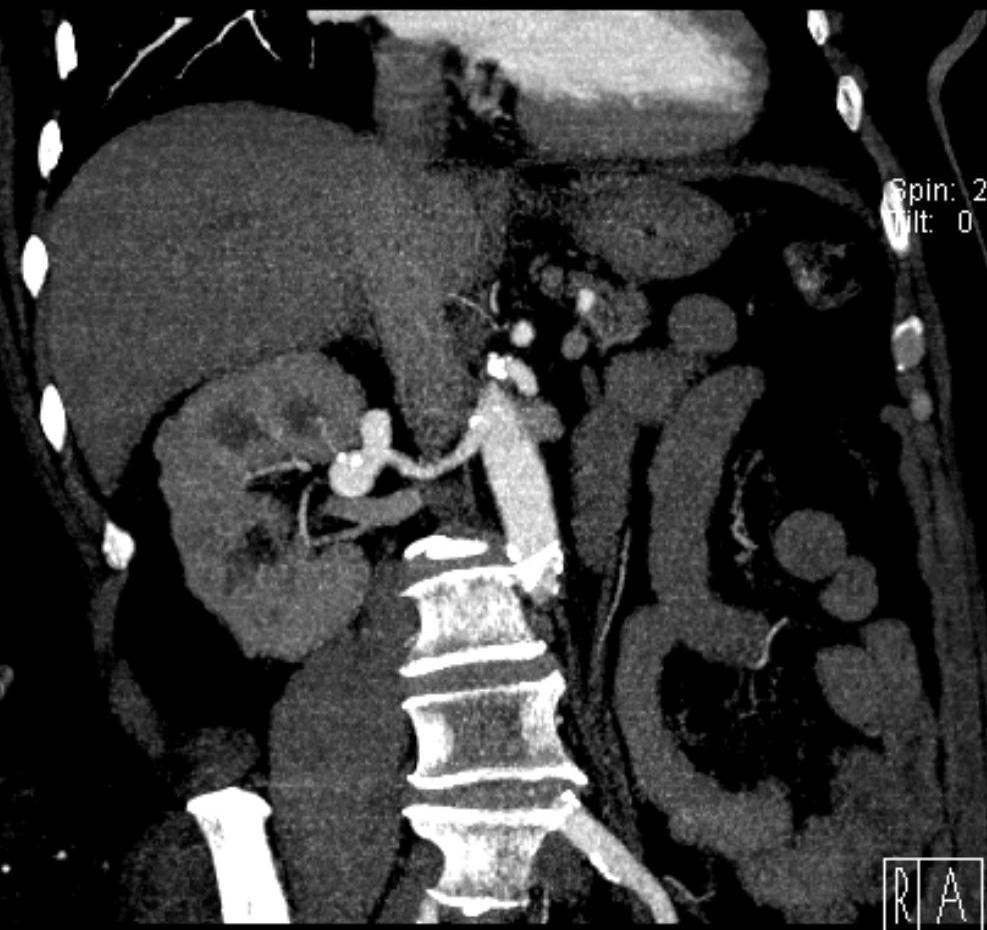
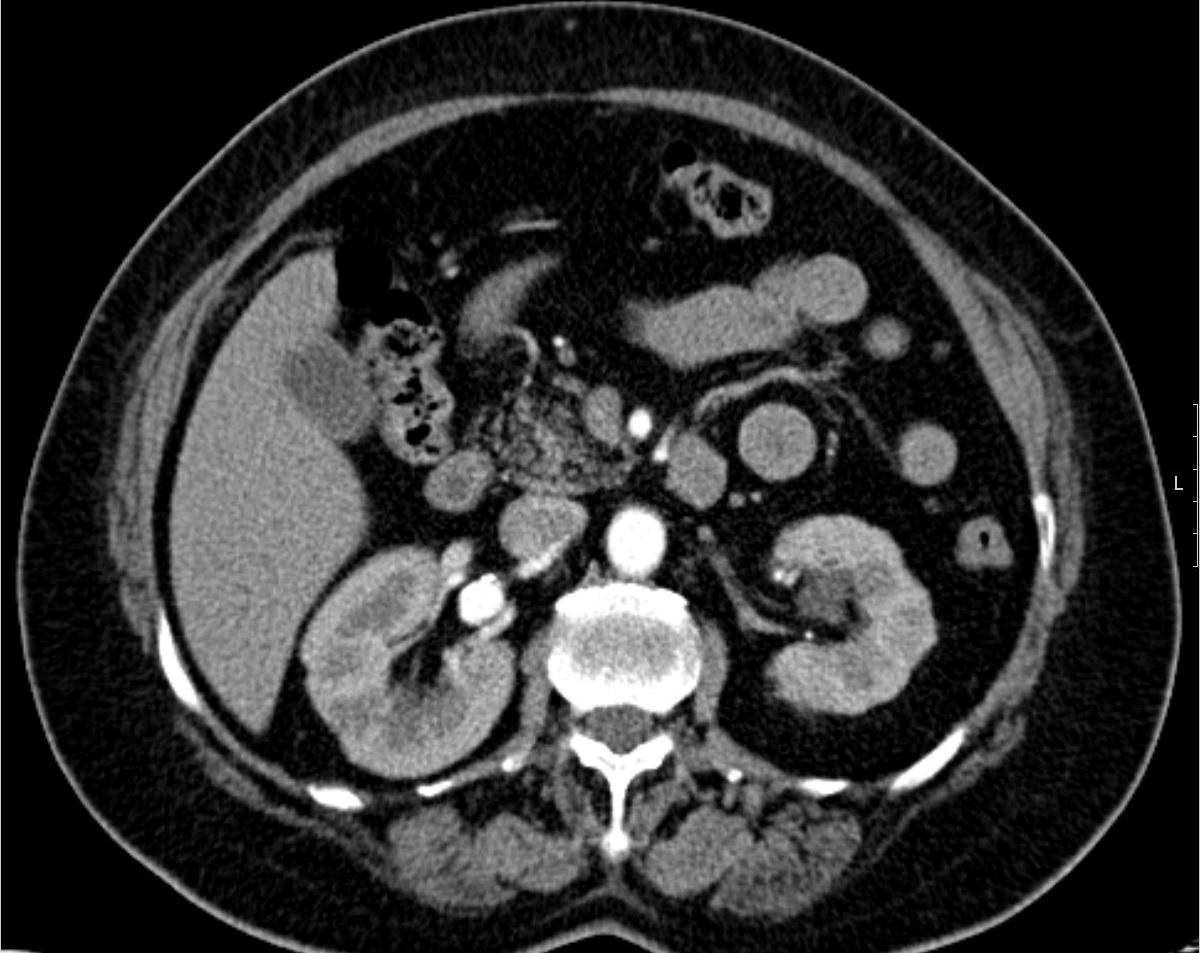
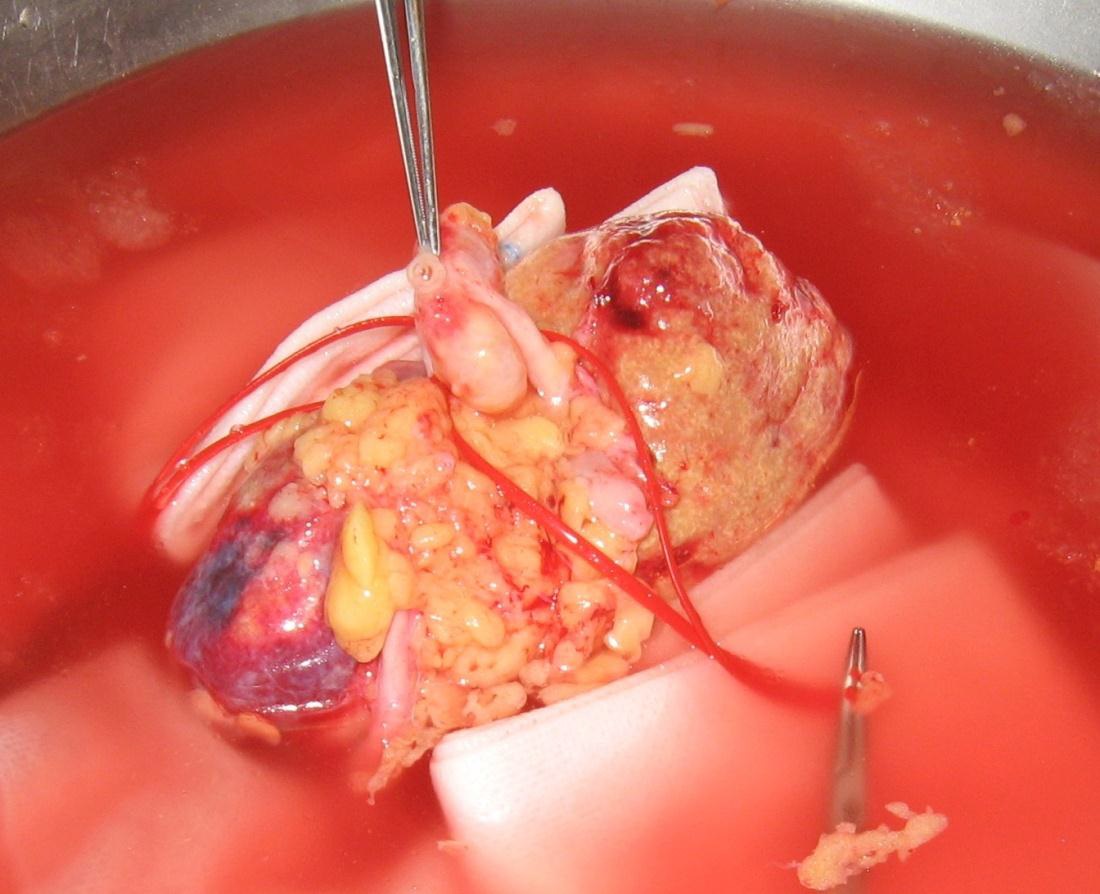
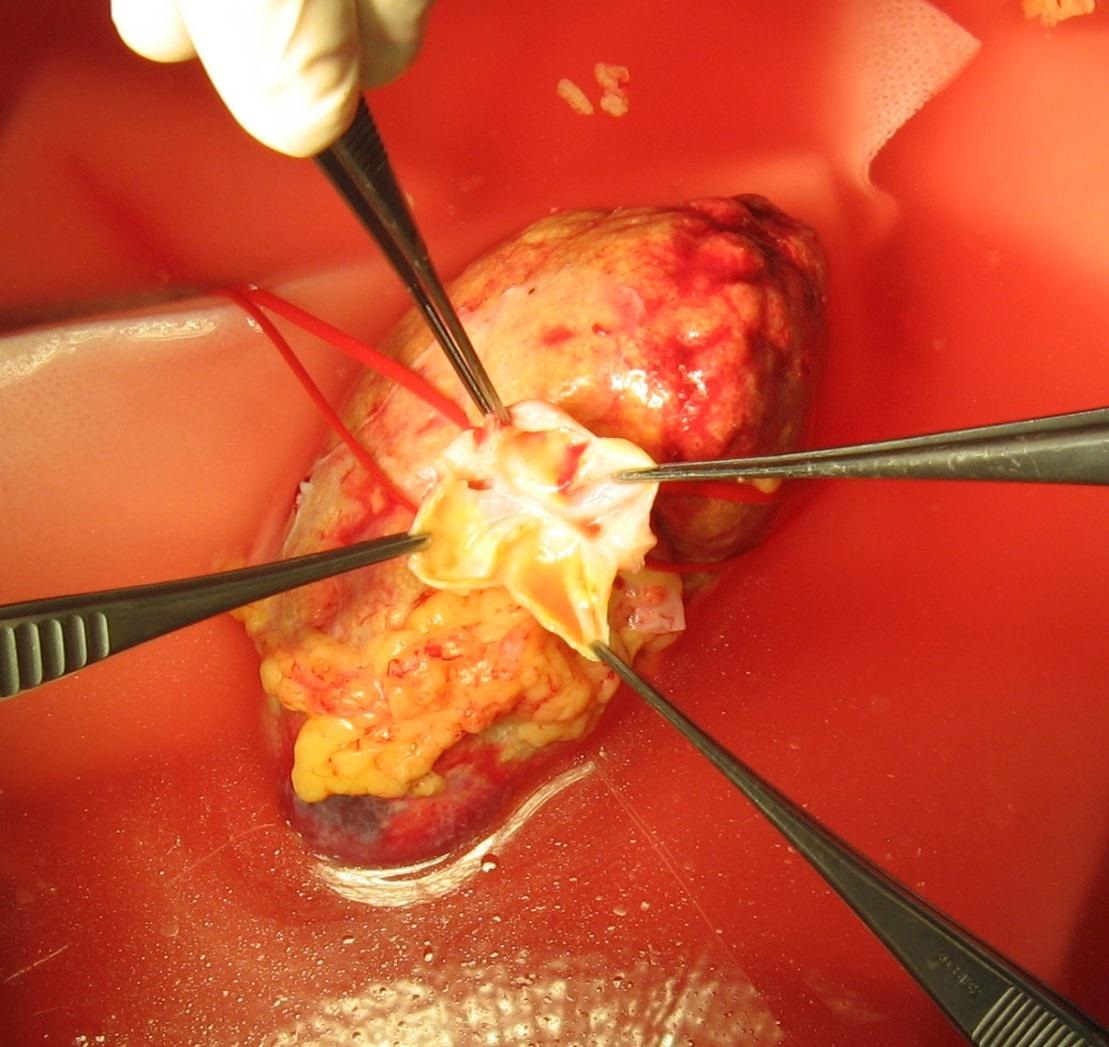
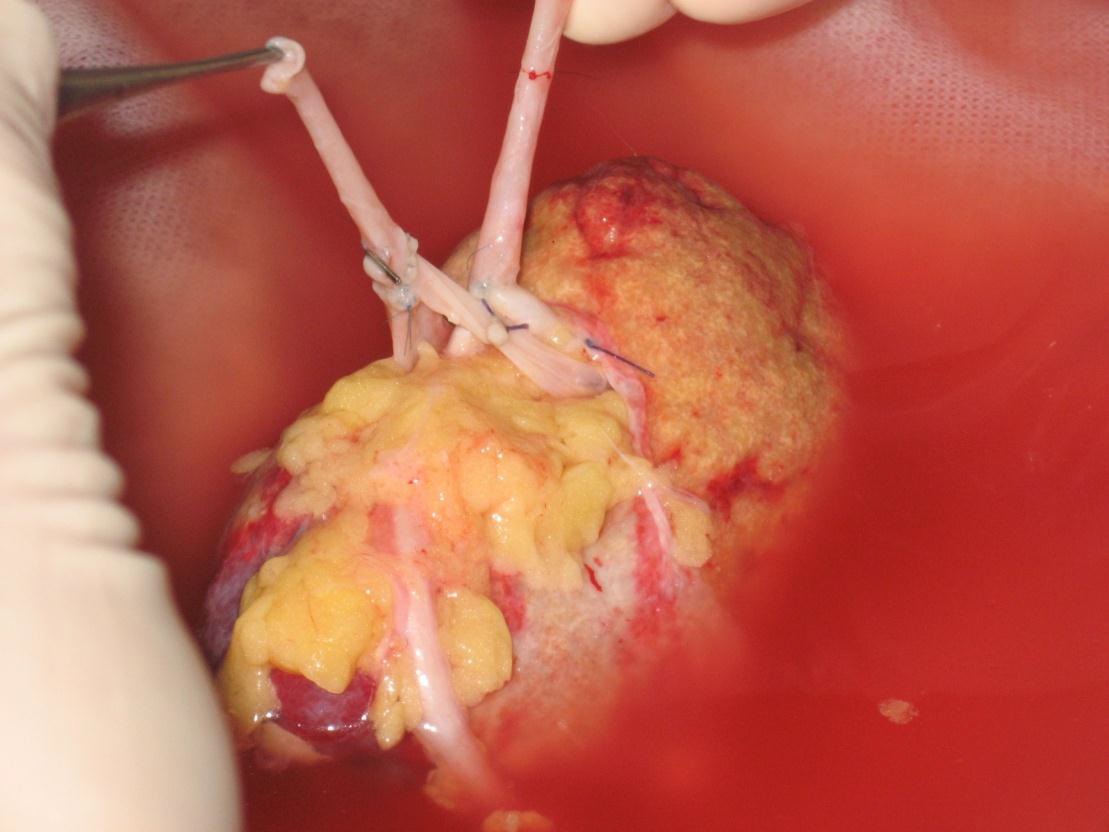
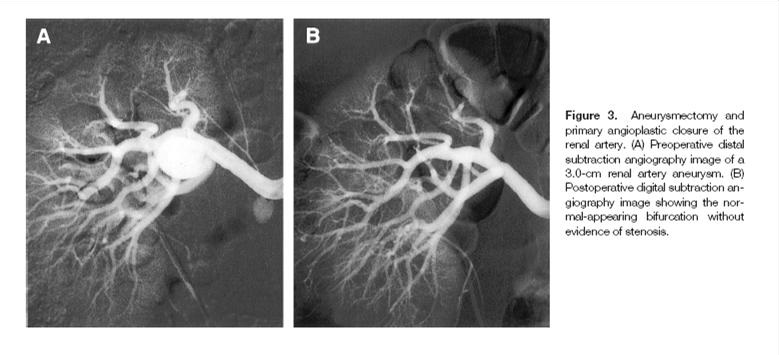
择期手术包括肾动脉瘤切除术后联合不同的血管肾血管重建包括血管局部修补,血管种植,旁路血管移植,体外修补后自体肾移植等,也包括肾切除或部分肾切除。
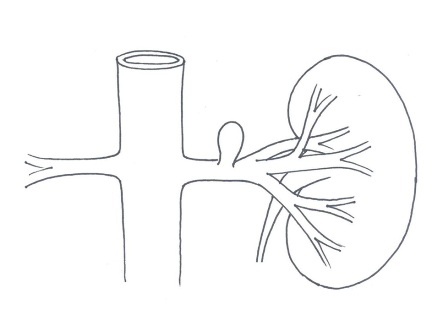 肾动脉主干假性动脉瘤示意图 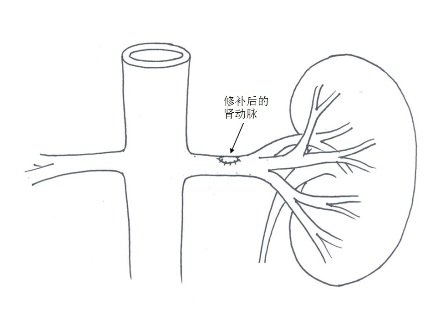 肾动脉主干假性肾动脉瘤修补术后示意图 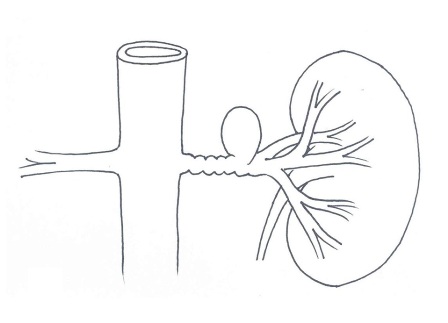
肾动脉瘤外科血管移植术前示意图
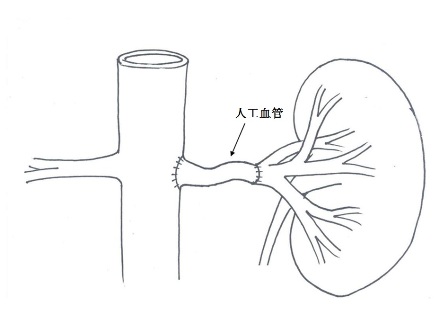 肾动脉瘤人工血管移植术示意图
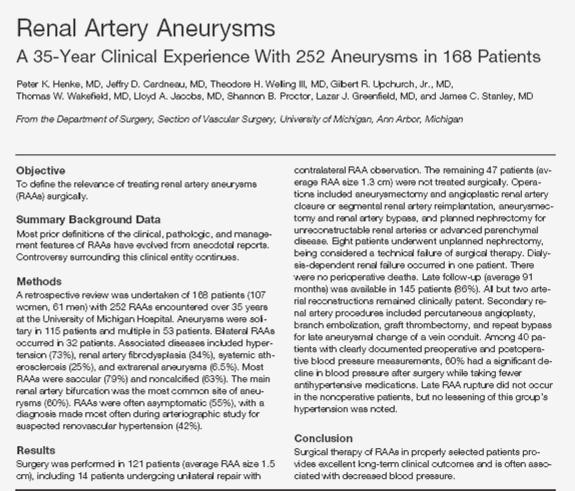
肾动脉瘤择期外科手术的并发症和死亡率非常低,很多作者报告几乎没有手术后的并发症和死亡率[2,32,33],有作者报告一例外科术后发生肾功能衰竭[37]。破裂动脉瘤的急诊手术的预后也已经大大的改善,文献显示已经从1949年前的62%,下降到1970年以后的6%。但妊娠期间肾动脉瘤破裂仍然有较高的死亡率。有报告,孕妇死亡率为56%,婴儿死亡率为78%[34]。
外科手术对于肾动脉狭窄伴有高血压的肾动脉瘤治愈率高达50~100%[32,33,35~37],尽管所报告的样本量较小,而且是单中心的,但外科对于肾动脉瘤的治疗似乎有长期效果。
一般来讲肾动脉瘤,特别是感染性动脉瘤由于出血和爆发败血症,可能有一个致命性的自然病史,同时可引起高血压和血尿,在过去大多数病例需要进行肾切除[27,28]。近年来,包括血管内支架,血管内栓塞作为简单、安全和有效的介入治疗在处理肾动脉瘤和肾实质动脉瘤浮出水面,可能作为外科治疗以外的选择之一[4~26]。详细情况本站另辟栏目专门介绍。
Endovascular treatment options
• Covered stents
• Coils
• Stent assisted coiling
• Glue or liquid embolics
• Flow diverters / multilayered stents
1. Cerny JC, Chang CY, Fry WJ. Renal artery aneurysms. Arch Surg 1968; 96: 653–663. 2. Stanley JC, Rhodes EL, Gewertz BL, Chang CY, Walter JF, Fry WS. Renal artery aneurysms. Significance of macroaneurysms exclusive of dissections and fibrodysplastic mural dilatations. Arch Surg 1975; 110: 1327–1333. 3. Hageman JH, Smith RF, Szilaghi DE, Elliott JP. Aneurysm of the renal artery: problems of prognosis and surgical management. Surgery 1978; 84: 563–572. 4. Henke PK, Cardneau JD, Welling TH et al. Renal artery aneurysm. A 35-year clinical experience with 252 aneurysms in 168 patients. Ann Surg 2001; 4: 454–463. 5. Klein GE, Szolar DH, Breinl E, Raith J, Schreyer HH. Endovascular treatment of renal artery aneurysms with conventional non-detachable microcoils and Guglielmi detachable coils. Br J Urol 1997; 79: 852–860.
6. 43. Wirthlin LS, Gross WS, James TP, Sandiq S. Renal artery occlusion from migration of stainless coils. JAMA 1980; 243:2064–2065.
18. Beaujeux R, Saussine Ch, Al-Fakir A et al. Superselective endovascular treatment of renal vascular lesions. J Urol 1995; 153: 14–17.
23. Tshomba Y, Deleo G, Ferrari S, Marina R, Biasi GM. Renal artery aneurysm: improved renal function after embolization. J End Ther 2002; 9: 54–58. 27. Ohebshalom MM, Tash JA, Coll D, Su LM, Schlegel PN (2001) Massive hematuria due to right renal artery mycotic pseudoaneurysm in a patient with subacute bacterial endocarditis. Urology 58(4):607 28. Hall CL, Cumber P, Higgs CM, Chalmers AH (1987) Life threatening haemorrhage from a mycotic renal pseudoaneurysm treated by segmental renal artery embolisation. Br Med J (Clin Res Ed) 294(6586):1526 29. Calligaro KD, Dougherty MJ. Renal artery aneurysms and arteriovenous fistulae. In: Rutherford RB, ed. Vascular Surgery. 5th ed. Philadelphia, Pa: WB Saunders; 2000:1697-702. 30. Love WK, Robinette MA, Vernon CP. Renal artery aneurysm rupture in pregnancy. J Urol. Dec 1981;126(6):809-11. 31. Sicard GA, Reilly JM, Rubin BG, et al. Transabdominal versus retroperitoneal incision for abdominal aortic surgery: report of a prospective randomized trial. J Vasc Surg. Feb 1995;21(2):174-81; discussion 181-3. 32. Dzsinich C, Gloviczki P, McKusick MA, et al. Surgical management of renal artery aneurysm. Cardiovasc Surg. Jun 1993;1(3):243-7. 33. Seki T, Koyanagi T, Togashi M, et al. Experience with revascularizing renal artery aneurysms: is it feasible, safe and worth attempting?. J Urol. Aug 1997;158(2):357-62. 34. Cohen JR, Shamash FS. Ruptured renal artery aneurysms during pregnancy. J Vasc Surg. Jul 1987;6(1):51-9. 35. Bulbul MA, Farrow GA. Renal artery aneurysms. Urology. Aug 1992;40(2):124-6. 36. Martin RS 3rd, Meacham PW, Ditesheim JA, et al. Renal artery aneurysm: selective treatment for hypertension and prevention of rupture. J Vasc Surg. Jan 1989;9(1):26-34. 38. 39. 40.
|