结肠癌是威胁人群健康的一个重要的社会问题。每年全世界将近有100万新诊的结肠癌病例,其中一半病人将会死亡。在欧洲和美国,每年新诊的结肠癌病例有30万,7—29%的患者来医院就诊时的首发症状为完全性或部分性肠梗阻[12,13],特别是左半结肠由于外压或内生性肿瘤引起的急性或亚急性肠梗阻,通常伴有恶心、呕吐、腹疼、腹胀和肠功能的改变[1,2]。结肠癌导致的急性肠梗阻属于外科急症,如果不治疗可以导致肠穿孔、败血症甚至死亡。传统的治疗手段是手术,手术的处理根据阻塞的位置、病变的范围。外科的姑息治疗包括结肠或空场造瘘或肠道旁路吻合。因为需要急诊手术,肠道未做准备情况下风险较大,并发症发生率在20~50%左右,30天死亡率达到30%[3,4]。 传统方法:在计划进行病灶切除前先行造瘘,减轻一期手术的并发症 为了减少急诊手术的并发症,通常情况下,患者将先予以结肠造瘘术,便于在可能的手术前清洁肠道。未来是否进行手术切除还取决于对原发灶进行疾病进行分期,也就是手术适应症的判定。如果适合进行手术,肠道准备后结肠癌患者的择期手术,并发症可从15-20%降至0.9-6%。并发急性大肠梗阻的结肠癌患者,5年生存率不到20%,比没有并发肠梗阻的患者预后要差很多。目前随着手术和围手术期管理的进步,一期手术切除和吻合的比例在日益增长,但仍只有40%左侧结肠癌并发肠梗阻的患者可以通过术中灌肠后行结肠次全切除。其余的患者则需要行暂时的或永久的结肠造口术。造口术相关并发症包括疼痛,皮肤刺激,回缩,疝出和狭窄。这些并发症的发生率在30~40%的病人[5,6]。这必然对患者的生活质量造成一定的影响[7~9]。
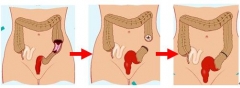
术前结肠梗阻段支撑架植入可以避免前期结肠造瘘,经过肿瘤分期和肠道准备后一期手术切除结肠病变
2. H.S. Chen and S.M. Sheen-Chen, Obstruction and perforation in colorectal adenocarcinoma: an analysis of prognosis and current trends, Surgery 127 (2000), pp. 370–376 3. K.J. Buechter, C. Boustany, R. Caillouette and I. Cohn Jr, Surgical management of the acutely obstructed colon, Am J Surg 156 (1988), pp. 163–168. 4. L.E. Targownik, B.M. Spiegel and J. Sack et al., Colonic stent vs. emergency surgery for management of acute left-sided malignant colonic obstruction: a decision analysis, Gastrointes Endosc 60 (2004), pp. 865–874. 5. J.A. Porter, E.P. Salvati, R.J. Rubin and T.E. Eisenstat, Complications of colostomies, Dis Colon Rectum 32 (1989), pp. 299–303. 6. J.J. Park, A. Del Pino and C.P. Orsay et al., Stoma complications: the Cook County Hospital experience, Dis Colon Rectum 42 (1999), pp. 1575–1580. 7. K.P. Nugent, P. Daniels and B. Stewart et al., Quality of life in stoma patients, Dis Colon Rectum 42 (1999), pp. 1569–1574. 8. R. Krouse, M. Grant and B. Ferrell et al., Quality of life outcomes in 599 cancer and non-cancer patients with colostomies, J Surg Res 138 (2007), pp. 79–87. 9. L. Sideris, F. Zenasni and D. Vernerey et al., Quality of life of patients operated on for low rectal cancer: impact of the type of surgery and patients' characteristics, Dis Colon Rectum 48 (2005), pp. 2180–2191. 10. Dohmoto M. New method - endoscopic implantation of rectal stent in palliative treatment of malignant stenosis. Endoscopia Digestiva 1991; 3: 1507-12 11. Tejero E, Mainar A, Fernández L, Tobío R, De Gregorio MA. New procedure for the treatment of colorectal neoplastic obstructions. Dis Colon Rectum. 1994 Nov;37(11):1158-9. 12. Boyle P. Some recent developments in the epidemiology of colorectal cancer. In: Bleiberg H, Rougier P, Wilke H-J, editors. Management of colorectal cancer. London: Martin Dunitz; 1998. pp. 19–34. 13. Ohman U. Prognosis in patients with obstructing colorectal carcinoma. Am J Surg. 1982;143:742–747. 14. Deans GT, Krukowski ZH, Irwin ST. Malignant obstruction of the left colon. Br. J. Surg. 1994; 81: 1270–6. 16. Tanaka T, Furukawa A, Murata K, Sakamoto T. Endoscopic transanal decompression with a drainage tube for acute colonic obstruction. Dis. Colon. Rectum. 2001; 44: 418–22. 17. Horiuchi A, Nakayama Y, Tanaka N et al. Acute colorectal obstruction treated by means of transanal drainage tube: Effectiveness before surgery and stenting. Am. J. Gastroenterol. 2005; 100: 2765–70. 18. Sumiyama Y, Saida Y. [Stent endoprosthesis and transanal decompression tube for colorectal obstructions.] Clin. Gastroenterol. 2005; 20: 1777–84. (in Japanese.) 19. Umpleby HC, Williamson RC. Survival in acute obstructing colorectal carcinoma. Dis. Colon. Rectum. 1984; 27: 299–304. 20. Khot UP, Lang AW, Murali K, Parker MC. Systemic review of the efficacy and safety of colorectal stents. Br. J. Surg. 2002; 89: 1096–102. 21. Baron TH, Harewood GC. Enteral self-expandable stents. Gastrointest. Endosc. 2003; 58: 421–33. 22. Suzuki N, Saunders BP, Thomas-Gibson S, Akle C, Marshall M, Halligan S. Colorectal stenting for malignant and benign disease: Outcomes in colorectal stenting. Dis. Colon. Rectum. 2004; 47: 1201–7. |