Portrait of Professor Paul Georges Dieulafoy, namesake of the Dieulafoy lesion. Open Source Image from the US National Library of Medicine.
French surgeon Paul Georges Dieulafoy(1839-1911),出生在图卢兹(法国),仙逝在巴黎。
Dieulafoy disease was first described by Gallard in 1884 as “miliary aneurysms of the stomach” and characterized in 1898 by Dieulafoy under the name “exulceratio simplex”
杜氏病定义:Dieulafoy病(国内称杜氏病)是一种胃粘膜下恒径动脉(caliber-persistent artery,CPA)畸形引起的出血,畸形的动脉直径通常为1~3mm,80%以上的Dieulafoy病发生于食管胃连接处的6cm之内的胃部,通常是在小弯侧,可能是由于这个区域的血液供应直接来源于胃左动脉,因而会出现这样粗管径的粘膜下动脉畸形。而胃的其他部位的血液供应来源于粘膜下血管丛的分支,这些分支的管径较小,故发生较粗管径动脉畸形的可能性较小(引自百度)。 胃恒径动脉综合症;Dieulafoy 血管畸形;Dieulafoy 粘膜糜烂;胃黏膜下恒径动脉破裂出血;粘膜下动脉畸形; Dieulafoy's lesion (exulceratio-形成溃疡 simplex Dieulafoy) is a medical condition characterized by a large tortuous arteriole in the stomach wall (sub mucosal) that erodes-侵蚀 and bleeds. It can cause gastric hemorrhage but is relatively uncommon. It is thought to cause less than 5% of all gastrointestinal bleeds in adults. It was named after French surgeon Paul Georges Dieulafoy, who described this condition in his paper "Exulceratio simplex: Leçons 1-3" in 1898.[2][3] It is also called "caliber-persistent artery" or "aneurysm" of gastric vessels. However, unlike most other aneurysms these are thought to be developmental malformations rather than degenerative changes.(维基百科) 什么是恒径动脉?(百度) 正常人胃壁供血主要依靠胃短动脉,其进入胃体后分支逐渐变细,在胃黏膜下形成毛细血管网。若胃短动脉到达黏膜下层血管内径没有逐渐变细而是保持恒定不变称恒径动脉。目前,一般认为恒径动脉属于先天性黏膜下血管发育异常。 发病部位
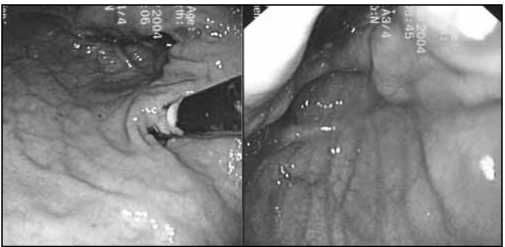
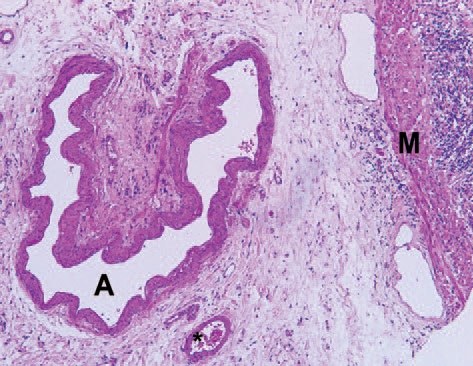
病理改变是什么? Dieulafoy 病的组织病理具有两个典型特征:病灶小,多呈2~5mm卵圆形浅表性糜烂,可深达黏膜肌层,在黏膜灶的中央可见直径1~3mm 动脉突出于黏膜缺损的部位,表面可有血栓附着,病灶周围黏膜无炎症改变,由于病灶小,内镜检查时易于忽视;位置特殊,Dieulafoy 病灶常位于胃贲门部小弯侧,Zanten 报道82%的病灶位于食管与胃连接的6cm 内,81%的病灶位于胃小弯侧,亦有极少数病灶位于十二指肠、空肠和结、直肠。  Dieulafoy 病的病灶在显微镜下的病理特征是: 1. 胃黏膜浅表性局灶性缺损伴有基底部纤维样坏死。 2. 在缺损的基底部有较大的动脉,动脉壁增厚;黏膜肌层有扭曲、增生的动脉。 3. 与黏膜肌层动脉伴随的静脉管径增粗。 高倍镜下可见破裂的动脉壁有轻度炎症反应,管腔内纤维血栓形成,动脉管壁黏膜下纤维沉着,胃黏膜肌层增厚,病灶周围黏膜无炎症反应。采用弹力纤维染色发现破裂动脉壁周围弹力纤维组织松解,动脉壁无瘤样扩张,亦无动脉炎的存在。Miko 分析了24 例Dieulafoy 病出血动脉与正常动脉的组织病理区别,发现Dieulafoy 病出血动脉有正常的组织结构,即由黏膜、肌层和外膜构成。黏膜下动脉管径正常,血管的增粗主要表现在黏膜肌层,动脉通过Wanken 弹力纤维固定于黏膜,动脉裂口处有黏膜缺损,伴随的静脉亦有破裂。 影像诊断: 从大量的网上和文献资料看,诊断都是来自胃镜发现出血的直接征象或粘膜表面有局限性血痂(血栓形成)。 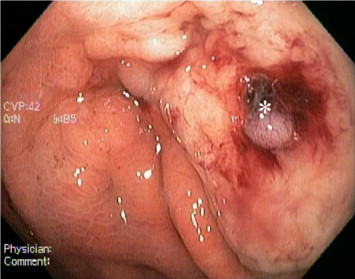 CT在诊断恒径动脉出血的角色还没有确定。
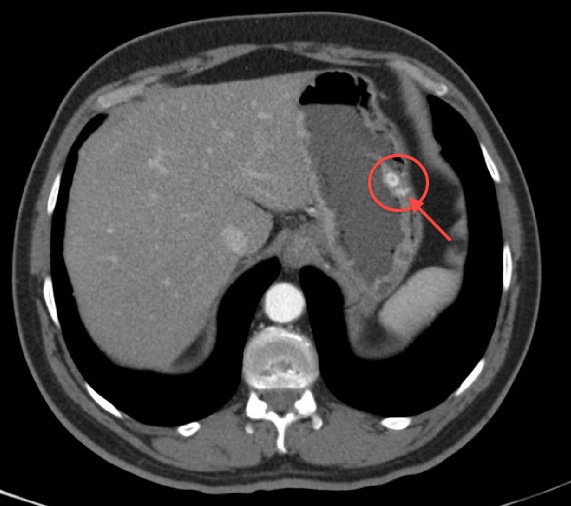
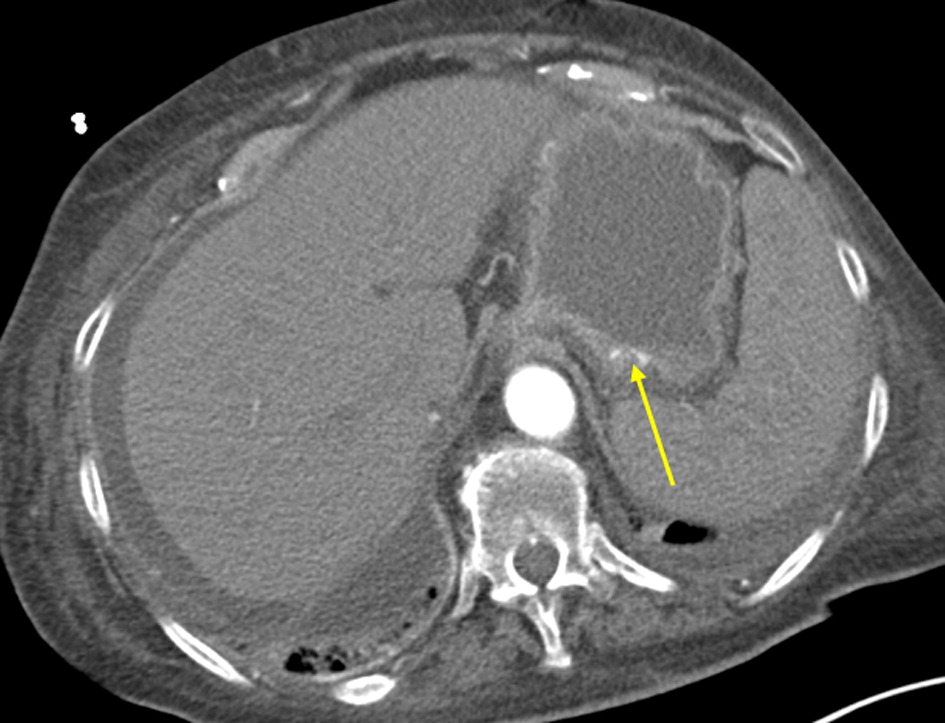
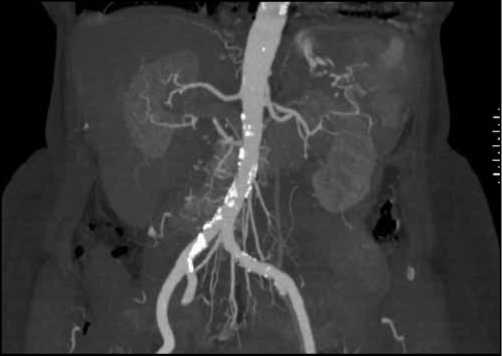
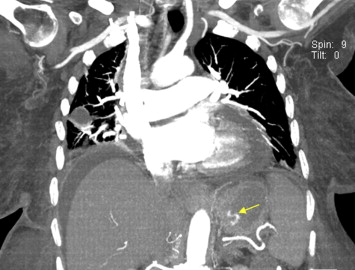 Coronal image from CTA of the chest obtained for suspected pulmonary embolism months prior to the admission for gastrointestinal bleeding shows a tortuous submucosal arteriole in the gastric fundus (yellow arrow). This finding corresponded in location to the Dieulafoy lesion found at endoscopy. Cardiomegaly, ascites, and right lung pneumonia are also present. 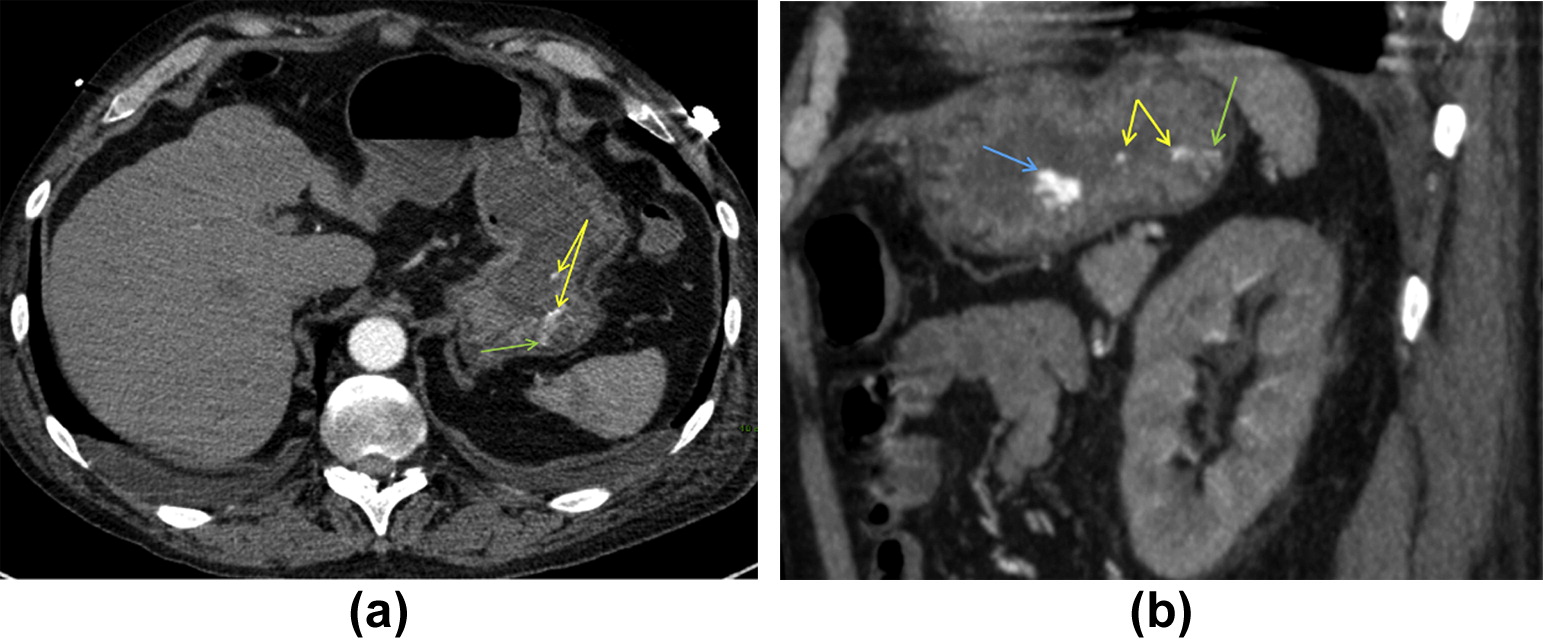 Contrast-enhanced images from CTA of the abdomen and pelvis obtained to look for the source of gastrointestinal haemorrhage. (a) Axial section in the arterial phase of enhancement shows an enlarged submucosal arteriole in the gastric fundus (green arrow) with small amount of active contrast medium extravasation seen in the lumen (yellow arrows). The finding corresponded in location to the Dieulafoy lesion subsequently found on endoscopy. (b) Sagittal reconstruction from the same CT examination shows the aforementioned Dieulafoy lesion (green arrow) and active contrast medium extravasation (yellow arrows), but also shows an additional radio-opaque focus within the gastric lumen, which was seen on the unenhanced CT sections and likely corresponded to recently ingested medication (blue arrow). 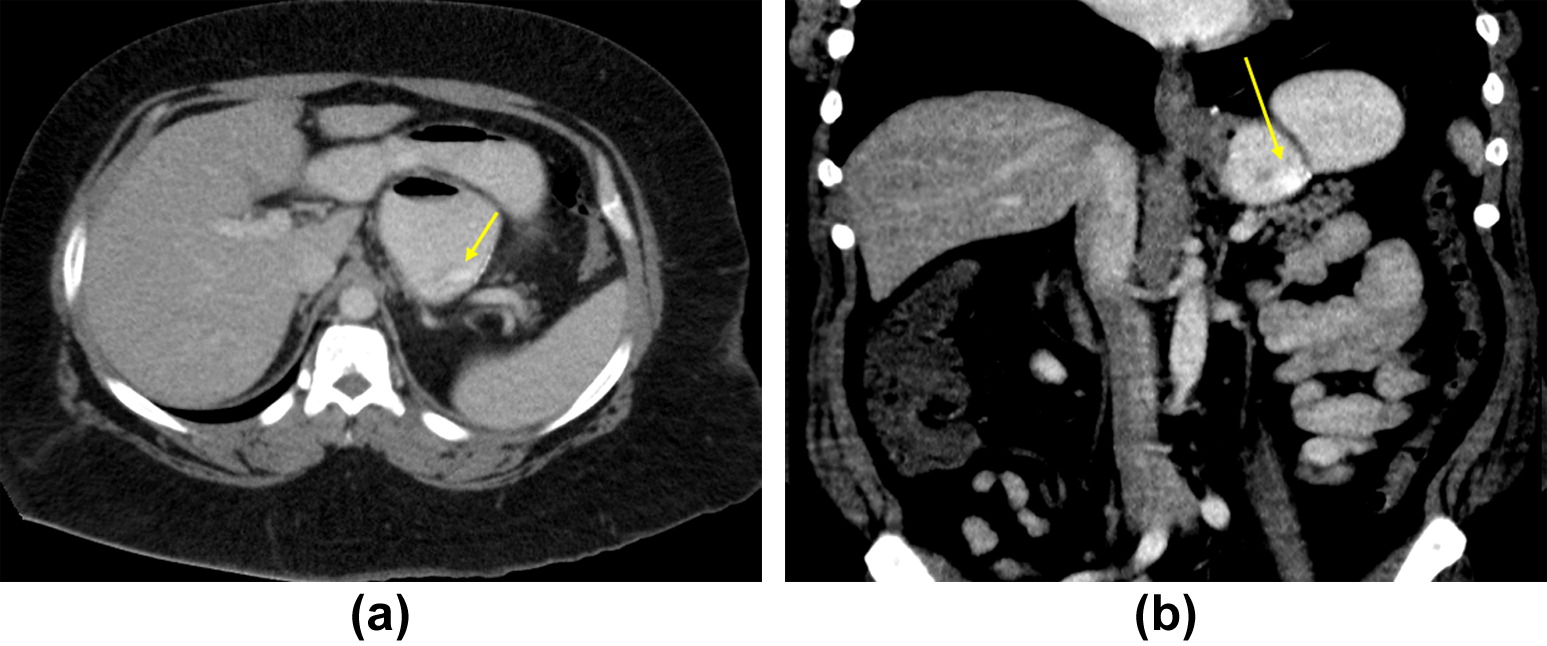
xial (a) and coronal (b) images from a CT examination of the abdomen with oral and intravenous contrast media obtained as part of the work-up for abdominal pain demonstrate a subtle linear area of increased enhancement in the posterior wall of the patient's gastric pouch near the staple line. This finding correlated in location with the Dieulafoy lesion seen on subsequent endoscopy.
CT诊断Dieulafoy 病的结论(Conclusion)
Near-definitive diagnosis of a Dieulafoy lesion can be obtained with enhanced CT of the abdomen. Optimal studies are performed in the arterial phase of intravenous contrast enhancement without administration of oral contrast material. CTA shows an enlarged submucosal arteriole in the gastrointestinal submucosal layer with or without active contrast medium extravasation into the lumen. Familiarity with the lesion and its manifestations can help guide radiologists to make the correct diagnosis in cases where endoscopy or standard angiography have failed. CT diagnosis can then help guide endoscopic and endovascular localization and treatment, ultimately improving patient outcomes.
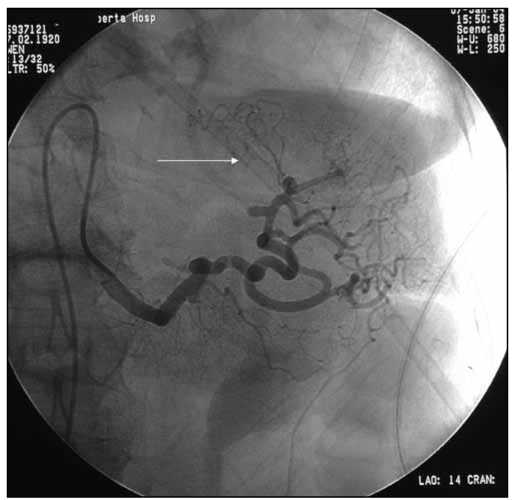
在Pubmed检索,没有找到几篇关于栓塞的文章
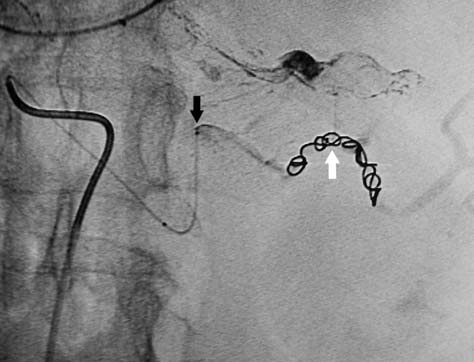
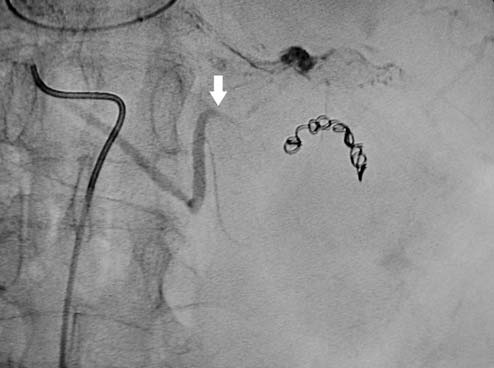
Alshumrani G1, Almuaikeel M. Angiographic findings and endovascular embolization in Dieulafoy disease: a case report and literature review. Diagn Interv Radiol. 2006 Sep;12(3):151-4.
究竟血管造影或介入放射学在消化道出血所扮演的角色主要是什么? 1. 出血的定位,主要为其它,特别是外科手术治疗提供线索 2. 在急性出血时,进行栓塞,缓解生命体征不稳定的状态,为进一步择期外科手术创造必要的条件 3. 作为一种治愈性的治疗手段,取代外科手术治疗 4. 作为一种治愈性措施,取代内镜的治疗 5. 仅仅作为其它治疗手段失败后的一种补救措施【1-3】 答案需要临床实践去证实,而且是大样本的实验,事实上对于一个罕见病来说,这几乎是不可能的。
1. Sam K. Kim, Vinay Duddalwar. Failed endoscopic therapy and the interventional radiologist: Non-variceal upper gastrointestinal bleeding. Tech Gastrointest Endosc 2005;7:148-155.
2. Ljungdahl M, Eriksson LG, Nyman R, Gustavsson S. Arterial embolisation in management of massive bleeding from gastric and duodenal ulcers. Eur J Surg 2002;168:384-90.
3. Poultsides GA, Kim CJ, Orlando R 3rd, Peros G, Hallisey MJ, Vignati PV. Angiographic embolization for gastroduodenal hemorrhage: Safety, efficacy, and predictors of outcome. Arch Surg 2008;143:457-61.
| ||||||||||||||||||||||||||||||||